Holiday Message from the Global RA Network
December 22, 2024

Rheumatoid arthritis (RA) is an autoimmune disease in which the body’s immune system mistakenly attacks its own healthy joints, causing chronic pain, stiffness, and systemic inflammation. It is a relatively common disease-approximately 1 in 100 people get it- and can significantly affect quality of life if not managed properly. Yet, with today’s array of effective treatments, people living with RA can strive toward better health outcomes and continue to pursue their personal and professional goals.
The way people with RA access and receive health care varies significantly across the EU and the Americas, particularly in rural and remote communities. This adversely affects people with RA as they depend on getting a timely and accurate diagnosis, fast access to rheumatologists, and appropriate public reimbursement for essential life-changing medications.
Each person living with RA is more than their diagnosis. They embody qualities of endurance, resilience, strength, and courage. At the Global RA Network (GRAN), we see these traits mirrored in our member organizations throughout Europe and the Americas—working hard together across borders to develop solutions that address unmet needs and advance RA care.
This past year, we broadened our efforts to deepen understanding of the everyday realities of RA patients. In 2024, building upon the insight gained from our ongoing data-gathering initiatives, GRAN continued to advocate for changing RA with healthcare providers, policymakers, and other stakeholders to implement approaches that address the daily challenges face by people with RA. By sharing these patient perspectives, we helped guide health policies, improve treatment strategies, and ultimately enhance care models. Our work continues to be guided towards a future where everyone affected by RA has equitable access to high-quality, patient-centered care.
This holiday season, we celebrate the progress we’ve made and look forward to the important work ahead. We warmly invite you—family members, friends, colleagues, and advocates—to join us. By staying informed and engaged, you can play a vital role in building a more hopeful future for all those living with RA.
To everyone living with RA around the world, we extend our wishes for a safe, healthy, and peaceful holiday season. We hope you’ll visit us in the coming months to learn how you can support our mission, ensuring that RA voices are heard, respected, and empowered in 2025 and beyond.
How Global RA Network members are honouring World Arthritis Day around the world
October 12, 2024

World Arthritis Day is a powerful moment for the millions living with rheumatoid arthritis (RA) to amplify their voices and be truly heard. RA isn’t just joint pain—it’s a life-threatening autoimmune disease that impacts every part of daily life, from mobility and work to mental health and relationships. For people living with RA, it often feels like an invisible battle, where timely diagnosis, access to proper treatment, and support are essential but often out of reach.
The Global RA Network is a collective of RA patient organizations across Europe and the Americas focussed on building international relationships and working on shared goals and to improve the lives of people living with RA.
During this year’s World Arthritis Day, Global RA Network member organizations are raising awareness, breaking down misconceptions, and advocating for the care and resources that can truly save lives. Explore our stories below to learn more about the urgent need for better care for this complex, debilitating disease that is a lifelong challenge that deserves everyone’s understanding, empathy and action.
Below are activities from our member organization happening in October.
Austria - Österreichischen Rheumaliga/Jung und Rheuma
1) Free Webinar on Psoriatic Arthritis
Tuesday, October 29th
Local time: 6:00 p.m. to 7:00 p.m.
Psoriasis or psoriatic arthritis, psoriasis is an autoimmune disease, as is rheumatoid arthritis, an inflammatory joint disease that occurs in about a third of people with psoriasis. Psoriatic arthritis can occur at any age, usually between the ages of 35 and 55. The disease occurs with approximately equal frequency in men and women. Click here to register.
2) Free Webinar on Personalized Rheumatism Therapy
Friday, October 18th
Local time: 6:00 p.m. to 7:00 p.m.
In his lecture "Personalized rheumatism therapy: Your genes inform you about effects and undesirable effects," Dr. Wöhrer will discuss the importance of genetic information in the treatment of rheumatism. He will explain how personalized medicine can help optimize the effectiveness of therapies and minimize undesirable effects. Click here to register.
Belgium - Reumatoïde Artritis Liga Vzw
The Imelda Hospital of Bonheiden and ReumaNet cordially invite you to the information morning 'Rheuma? Action!' on Saturday 19 October 2024 from 9 am. The program is filled with presentations and workshops of your choice.
Everyone is welcome, participation is free. You do need to register. You can do that here (click here).
Do you have any questions? Then you can contact ReumaNet via info@reumanet.be
Brazil - Grupo de Pacientes Artriticos de Porto Alegre -RS
Senior month is already knocking on the Door, along with the month of October, raising awareness about rheumatic diseases.. Here's a sneak peek of what's coming up for our month of October!!

Canada – Arthritis Consumer Experts
On #WorldArthritisDay, Arthritis Consumer Experts is sharing their recently published #ACESurvey result on arthritis and private health insurance. Private health insurance is a cornerstone of healthcare access for millions of Canadians, providing coverage for medications, physical therapy, and other essential services.
The findings of the National Survey on Private Health Insurance are critical for understanding how well private health insurance plans meet the needs of people with arthritis and identifying areas for improvement. In this special edition of JointHealth™ insight, ACE breaks down the Survey findings into key sections, each addressing an essential aspect of the insurance experience for arthritis patients.

Chile - Fundación Me Muevo
As a foundation, they focus on creating a community of support for people living with Rheumatoid Arthritis and raising awareness of the disease. Every October, they launch #OctubreArtritis, because the 12th of this month is World Arthritis Day. This month they focus on informing, fighting or sharing activities related to Rheumatoid Arthritis with true and reliable information. They also want to update the status of the country's situation regarding coverage and access to RA. In addition, #OctubreArtritis has a social purpose, by calling for support from those close to them and Chilean society in the fight against the disease, accompanying patients and eliminating doubts regarding Rheumatoid Arthritis.
Join them through their social networks and website to stay up to date with the campaigns. Be part of the community! Click here to learn more.
Chile - Red ASOPAN (Pan American Network of Associations of Rheumatic Patients) - Latin and South America
Arthritis 2.0” represents a new perspective on your disease, in which arthritis is no longer seen as a debilitating condition, and transforms into an opportunity for more effective and empowering management. With advancements in technology, research, and therapies, patients can access personalized treatments, leverage digital tools to monitor their health, and actively participate in symptom management. This “new face” of arthritis also means a more holistic approach that includes mental, social, and physical well-being, providing hope for a better quality of life and greater treatment options.
Watch testimonial videos on their Facebook page and Instagram page.

Crete – Arthritis Foundation of Crete
In the context of World Arthritis Day, the Arthritis Foundation of Crete organized actions in various cities, including: Thessaloniki, Patras, Heraklion, and Chania
Let's come together to raise awareness about arthritis in the community, share experiences and support one another!
Learn more: www.srcrete.gr
Cyprus – Cyprus League Against Rheumatism
On the occasion of World Rheumatism Day, the Cyprus Association of Rheumatologists
(SyReK), invites you to participate in the event "Walk with Rheumatologists" on Saturday, October 12. The event will take place at 4:00 p.m. on the Finikoudes pedestrian street in Larnaca (starting from Europe Square), with the slogan "Wear me, always with pride", inviting the public to wear the Association's anniversary bandana and walk next to the rheumatics, supporting their struggle.
The campaign aims to inform and raise awareness among society and relevant agencies about the challenges faced by people with rheumatic diseases in their daily lives. The event "Walking with Rheumatoid Patients" is organized by SyReK under the auspices of the Mayor of Larnaca, Mr. Andreas Vyra, who will announce the start of the symbolic march at 5:45 p.m. in Europe Square.
Learn more: https://bit.ly/3Y0weyd
France - AFLAR (French League Against Rheumatism)
AFLAR will be present at the 27th Edition of LA PARISIENNE. Information workshops on women's health, osteoporosis and physical activity will be offered and documentation on osteoporosis is available on the stand.
Friday October 18, Saturday October 19 and Sunday October 21
Location: Stade Emile Antoine, 75007 Paris
Learn more: https://la-parisienne.net/
Ireland – Arthritis Ireland
The theme for World Arthritis Day 2024 (October 12th) is 'Knowledge is Power, informed choices, better outcomes’. World Arthritis Day 2024 emphasises the importance of access to information, especially in our fast-paced digital age where individuals with arthritis are inundated with vast amounts of data to process.
Arthritis Ireland’s STEPS programme - Steps Towards Empowered People - is a unique, tailored initiative designed to prioritise the needs of individuals living with arthritis. It equips individuals with the knowledge and tools necessary to make informed decisions about their health journey.
Whether you are newly diagnosed or have been living with arthritis for some time, you can learn more about the STEPS programme and how to get involved by clicking here.
Italy - Associazione Nazionale Persone con Malattie Reumatologiche e Rare (APMARR)
From 17 to 19 October the third National Congress of the Italian Society of Pediatric Rheumatology - REUMAPED will take place in Lecce, in which APMARR will also participate.
In particular, from 8:45 to 11 am on Saturday, October 19, the session “Medical-patient-caregiver communication “the families at the center” will take place in order to deepen and discuss this very important topic.
The session will take place in the Sybar Room Hilton Garden Inn, and you can participate both physically and remotely by registering here.

Netherlands - ReumaZorg Nederland
Webinar invitation on 14 October: Sjögren, systemic lupus and scleroderma
Are you dealing with scleroderma, Sjögren's syndrome or systemic lupus? These forms of systemic rheumatism not only affect joints, but they can also affect organs, skin and glands.
In order to draw more attention to these invasive conditions, they are hosting a webinar on Monday 14 October from 7pm to 8pm. Guest Speaker is Dr. Madelon Vonk, rheumatologist at the Radboudumc and specializes in research into systemic rheumatism. Click here to learn more.
Poland - 3majmy się razem
On October 10 in the Parliament of the Republic of Poland, the National Association of Young People with Inflammatory Connective Tissue Diseases "3majmy się razem" celebrated the opening of the exhibition "Dapasowani".
The exhibition aims to draw attention to the challenges faced by patients with inflammatory spondyloarthropathy, a group of rheumatic diseases that cause inflammation of the joints and spine. Currently, there is no effective therapy, and treatment focuses on relieving pain, improving mobility and preventing complications.
The exhibition #Dopasowani tells the stories of patients who, thanks to education and modern treatment, can lead active and fulfilling lives, pursuing their passions and functioning in society.
Learn more: https://3majmysierazem.pl/
Serbia - Udruženje obolelih od reumatskih bolesti Republike Srbije (ORS)
The Association of Rheumatic Diseases of the RS (ORS), like every year, joins EULAR in marking the World Arthritis Day on October 12, 2024 at the Central Office in Belgrade, branches of the ORS in Niška Banja, Novi Sad , Kragujevac, Užice, with the aim of reminding the general public in the RS, health professionals, and state institutions of how important it is to enable arthritis sufferers to receive an early diagnosis, modern treatment, and support in the fight against the disease, in order to preserve occupational and reproductive health, social well-being and health-related quality of life improvements. Click here to learn more.
Spain – ConArthritis
On the occasion of the celebration of National Arthritis Day, which will take place on October 12, they are launching, once again, the campaign “October, arthritis and spondyloarthritis month” to raise awareness of a group of rheumatic diseases such as juvenile idiopathic arthritis, psoriatic arthritis, rheumatoid arthritis and spondyloarthritis, which affect more than one million people in Spain.
They also encourage you to wear green this Saturday and share your photo with the hashtag #Vendeverde24. Will you join this action to raise awareness about arthritis and spondyloarthritis? #OctAR24
Click here to learn more.
United States of America - International Foundation for Autoimmune & Autoinflammatory Arthritis
World Arthritis Day is a vital opportunity to shine a light on the challenges faced by those living with arthritis and RMDs. By raising awareness, promoting early diagnosis and treatment, and empowering individuals with accurate information, we can make a significant difference in the lives of millions. Let’s come together this October 12th to support and advocate for those affected by these conditions. Click here to learn more.
EULAR 2024 Recap
June 28, 2024

The European Alliance of Associations for Rheumatology, EULAR, held its 2024 Congress, June 12-15 in Vienna, Austria, featuring the world’s leading experts in rheumatology sharing the latest groundbreaking research, clinical innovations, and advancements in arthritis patient care.
EULAR 2024 Congress featured an extensive programme, including more than 130 scientific sessions, 2 dedicated EULAR Recommendations Sessions, and over 1000 abstract presentations covering the latest in rheumatology research and practice.
Here are key research studies on rheumatoid arthritis and other key arthritis topics from EULAR 2024:
New research on rheumatoid arthritis
Measuring the impact of lifestyle intervention in RA
Title of study: Long-term Effectiveness of a Lifestyle Intervention for Rheumatoid Arthritis: Two-year follow-up after the “Plants for Joints” randomised clinical trial
Background
EULAR has recommended in the past lifestyle changes for people with inflammatory arthritis, including rheumatoid arthritis (RA).1 Managing RA typically involves medications, but lifestyle changes play a crucial role in improving symptoms and supporting physical and emotional health. The 16-week "Plants for Joints" (PFJ) program focuses on a whole-food plant-based diet, physical activity, and stress management. The goal of this study was to assess the long-term effectiveness of the PFJ lifestyle intervention on RA disease activity two years after the program ended.
Study details
- Studied the effects of a lifestyle intervention on people with RA.
- Participants followed a whole-food, plant-based diet, did physical activity, and practiced stress management.
- The trial compared these participants to those receiving usual care.
- Evaluated the long-term effectiveness of the intervention, specifically with regards to disease activity after 2 years.
- Those who had low disease activity (DAS28 <2.6) were given a plan to possibly reduce their medication with their rheumatologist's guidance. Changes in medication were classified as "increase", "stable", or "decrease".
- Monitored other health markers like weight, cholesterol, and inflammation.
Findings
Specific improvements were seen in the number of tender joints and general health. About 65% of participants had better DAS28 scores with stable or reduced medication. HDL cholesterol (the "good" cholesterol) increased, and CRP (a marker of inflammation) remained lower than baseline levels. However, there were no significant changes in weight, waist circumference, LDL cholesterol (the "bad" cholesterol), or HbA1c (a measure of blood sugar control).
Key takeaways
- The PFJ program led to long-lasting improvements in RA symptoms, which were maintained two years after the intervention. A significant number of participants were able to reduce their RA medication while maintaining or improving their disease activity (DAS28) scores.
- The study showed adopting a whole-food plant-based diet, regular physical activity, and stress management can significantly improve RA symptoms and overall health.
- Continuous support through biannual visits and webinars also helped participants adhere to the lifestyle changes, contributing to sustained benefits.
Click here to learn more about the study.
Reference
- Gwinnutt JM, et al. 2021 EULAR recommendations regarding lifestyle behaviours and work participation to prevent progression of rheumatic and musculoskeletal diseases. Ann Rheum Dis 2023;82:48–56
Patterns of pain in early rheumatoid arthritis: New Insights
Title of the study: Dissecting early RA patient trajectories through time-independent disease state identification identifies distinct patterns dissected by inflammation in blood or joints.
Background
This study explores different patterns of pain in patients with early RA. Understanding these patterns is important for improving treatment and management of the disease.
Study details
The study focussed on non-articular pain – an issue which is common in early RA and associated with lower remission rates.2 Non-articular pain refers to pain that originates from structures outside of the joints. This type of pain does not come from the joint itself but from other tissues such as muscles, tendons, ligaments, or bones.
Researchers analyzed data from patients with early RA to identify different pain patterns at the start and over 12 months
Findings
The study included over half of the patients reporting non-articular pain, with a focus on pain in certain regions of the body and on widespread pain. At the start, more than half of the patients reported non-articular pain, mostly in regional areas. The most common pain patterns were in the axial region (34%), both upper quadrants (20%), and both lower quadrants (10%). Over a year, 42% of patients with regional pain saw it persist or worsen, while 73% of those with widespread pain saw improvement. Joint inflammation was often found in the same areas as non-articular pain and persisted over time.
Key takeaways
Non-articular pain is common in early RA and often continues in the first year after diagnosis. RA activity may contribute to the persistence of pain in these areas. Early intervention to prevent and treat non-articular pain is recommended.
Click here to learn more about the study.
Reference
- Bykerk VP, et al. Regional and widespread patterns of non-articular pain are common at RA diagnosis and contribute to poor outcomes at 12 months. Ann Rheum Dis 2020;79(Supp1):585
Exploring the link between dental health and RA
Title of the study: Is tooth extraction as proxy for periodontal disease related to the development of RA? Lessons from a longitudinal study in the at-risk stage of clinically suspect arthralgia
Background
Researchers wanted to see if dental health issues, like tooth extraction, might be linked to developing inflammatory arthritis.
Study details
- Included 700 people with early joint pain, a condition known as clinically suspect arthralgia (CSA).
- 96 people tested positive for Anti-Citrullinated Protein Antibodies (ACPA), an antibody that is a marker for RA and can help in diagnosing the disease.
- 121 people eventually developed inflammatory arthritis.
- Focused on 206 patients who had dental extractions (many of whom were older, smokers, with higher body mass index (measure of body fat based on height and weight that applies to adult men and women), and more early joint inflammation.
Findings
Tooth extraction was linked to a higher chance of developing arthritis, but only in those with the ACPA antibody. This link was strong regardless of income or visible joint inflammation on MRI scans.
Key takeaways
Taking care of your teeth might help lower the risk of developing inflammatory arthritis, especially for people at risk for inflammatory arthritis.
Click here to learn more about the study.
Predicting treatment response in patients who have not started medication for their RA
Title of the study: Multi-modal analysis of synovial tissue macrophages informs on treatment response in naive to treatment Rheumatoid Arthritis
Background
New research presented at the 2024 EULAR congress looks at using multi-modal analysis to predict how patients with rheumatoid arthritis (RA) will respond to treatment. Multi-modal analysis is a way of looking at different types of information together to get a complete understanding of a situation. For an arthritis patient, it means doctors and researchers use various kinds of data to understand the disease better. This can include:
- Medical tests (for example, results from blood tests, X-rays, and MRI scan)
- Patient reports (for example, information from patients about their symptoms and how they feel)
- Lifestyle information (for example, details about diet, exercise, and daily activities)
This study aims to find biomarkers that can help doctors decide the best treatment for each patient.
Biologic markers, commonly termed “biomarkers,” are substances in the body (for example, blood or joint fluid) that can be measured and inform patient conditions and assist with early diagnosis, optimization of treatment and disease monitoring.
Study details
Researchers studied the synovial tissue, which lines the joints, in patients with RA who had not yet received treatment. They used advanced techniques to analyze inflammation and identify specific immune cell markers. The goal was to see if these markers could predict how well patients would respond to conventional RA treatments.
Findings
The study found that certain types of immune cells in the joint tissue are linked to how well patients respond to treatment. This suggests that analyzing these cells can help doctors predict which treatments will work best for different patients.
Key takeaways
Using multi-modal analysis to study joint tissue can improve treatment decisions for RA patients. This approach can help doctors choose the best treatment early, leading to better outcomes for patients.
Click here to learn more about the study.
Other important studies presented at EULAR

Raising our voice: Arthritis patients participating in research
Title of study: Myths vs Realities: An honest feedback from the scientific community on collaboration with patients partners in the NECESSITY research project
Background
Are patient partners a necessity in research? This is a question the EULAR community has answered by recognizing the importance of involving patients in developing recommendations. The role of patients in research is growing but still new in Europe. At the 2024 EULAR congress, researchers presented survey data highlighting the scientific community's views on involving patients in research for Sjögren’s disease.
Study details
Researchers conducted a survey to understand the views of scientists on involving patients in research focused on primary Sjögren’s disease, an autoimmune disorder causing dry eyes and mouth, fatigue, pain, and other complications. While treatments exist for symptoms, there are no cures. The survey collected feedback from the scientific community about the necessity and impact of patient partners in research.
Findings
The survey showed that scientists see value in involving patients in research. They believe that patient partners can offer unique insights and help develop better treatments.
For example, a majority of respondents favoured working with patients to validate unmet needs – especially those around symptoms and care expectations. Over 95% of respondents stated they would be willing to seek out patient partners in the future and view them as genuine research partners.
Key takeaways
Involving patients in research is seen as beneficial by the scientific community. This collaboration can lead to better outcomes and more effective treatments. As this practice evolves, it is essential to continue exploring its benefits and challenges to make the most of patient involvement in research.
Click here to learn more about the study.
Title of study: EULAR recommendations for the involvement of patient research partners in rheumatology research: 2023 update Annals of the Rheumatic Diseases
Background
In 2011, EULAR published the first recommendations on involving patient representatives in scientific projects. These recommendations defined the role of patient research partners (PRPs). Since then, the role of PRPs has evolved, and their involvement in research has shown many benefits. PRPs are patients who actively participate in research projects, providing valuable insights based on their experiences.
Study details
- EULAR formed a task force consisting of 13 researchers, 2 health care professionals, and 10 PRPs.
- Conducted a literature review to gather current information on the role and definition of PRPs.
- Focused on improving recruitment, selection, and monitoring processes for PRPs. The study aimed to enhance the integration of PRPs into research teams on an equal basis with professional researchers.
Findings
The updated recommendations highlight the importance of involving PRPs in research beyond just being study participants. PRPs contribute to guideline development, clinical research, patient-reported outcomes, patient preference studies, research grant applications, regulatory processes, and international research consortia. Their involvement ensures that patient perspectives are included in all aspects of research.
Key takeaways
Involving PRPs in arthritis research is crucial for developing patient-centered outcomes and ensuring that research reflects patient needs and preferences. The updated EULAR recommendations provide a framework for effectively recruiting, selecting, and integrating PRPs into research teams. This approach will enhance the quality and relevance of arthritis research, ultimately benefiting patients.
Click here to learn more about the study.
Using digital health tools to assist patient self-management
Title of the study: A cognitive behavioural digital health application is effective in improving psychological quality of life in patients with rheumatoid arthritis
Background
This study looks at how a digital health app using cognitive behavioral therapy (CBT) can improve the quality of life for patients with rheumatoid arthritis (RA).
CBT is a type of psychological treatment that helps people understand the thoughts and feelings that influence their behaviors. It is commonly used to treat a variety of mental health conditions, including depression, anxiety, and stress.
Study details
RECLARIT is a digital health app designed for people with RA. The app provides methods and exercises – often relying on cognitive behavioural therapy – and follows a holistic approach to support people to enhance their mental quality of life. The app aims to provide self-management advice and support, empowering patients to take control of their disease and improve their overall well-being.
To show that digital health tools are effective, researchers conducted a study using RECLARIT to help RA patients manage their condition. The study included a diverse group of participants who used the app to receive psychological support and self-management resources.
Findings
The study found that the app significantly improved the psychological quality of life for RA patients. These positive effects were maintained over several months, showing the app's long-term benefits.
Key takeaways
Using a cognitive behavioral digital health app can improve the quality of life for RA patients. Incorporating self-management advice and digital resources into routine care can empower patients and enhance their overall care experience. Further development and use of such digital health tools could greatly benefit patients with chronic diseases like RA.
Click here to learn more about the study.
References
- Solomon, D.H., Rudin, R.S. Digital health technologies: opportunities and challenges in rheumatology. Nat Rev Rheumatol16, 525–535 (2020). https://doi.org/10.1038/s41584-020-0461-x
- Schäfer, C., & Keyßer, G. (2022). Lifestyle Factors and Their Influence on Rheumatoid Arthritis: A Narrative Review. Journal of clinical medicine, 11(23), 7179. https://doi.org/10.3390/jcm11237179
Title of study: Determinants of Digital Health Technology Use in Rheumatology Care - Secondary Analysis of Data from A Survey Among German RMD-Patients
Background
Digital health technologies (DHTs) are tools like mobile apps and wearable devices that help patients understand their symptoms and self-manage their conditions. These technologies continue to become more common in arthritis care. To understand why some patients use these technologies and others do not, a study in Germany surveyed 337 patients who receive rheumatology care.
Study details
- Data was analyzed separately for men and women and for two age groups: those younger than 55 years and those 55 years and older.
- Over half of the patients (55%) used DHTs.
- Average age of the patients was 52.5 years.
Findings
Factors associated with NOT using DHTs
- Believing DHTs offer no real benefits.
- Not using specific digital therapeutic apps designed for rheumatology.
- Issues with internet or network coverage.
- Being satisfied with current non-digital methods and seeing no need for DHTs.
Factors associated with using DHTs
- Using wearable devices for rheumatology before the COVID-19 pandemic.
- Being open to the idea of video consultations.
- Having an optimistic attitude towards digital healthcare since the COVID-19 pandemic.
- Flexibility that DHTs offer.
- Using other health-related mobile apps before the pandemic.
Key takeaways
- COVID-19 impact: The pandemic has encouraged more patients to try digital health technologies.
- Diverse Needs: There is still a significant group of patients who prefer traditional, non-digital methods.
- Comprehensive Care: Offering both digital and traditional options ensures that all patients’ needs and preferences are met, making rheumatology care more inclusive.
Click here to learn more about the study.
Launch of EULAR Projects

Survey Now Open: EULAR Invites Patients Across Europe to Participate in Groundbreaking Study on Rheumatic and Musculoskeletal Diseases
Background
EULAR has launched a new survey to gather important insights from patients across Europe on the impact of rheumatic and musculoskeletal diseases (RMDs). This survey aims to improve the understanding and care of these conditions by collecting data directly from those affected.
The survey is available online and will soon be accessible in multiple European languages. It invites people living with RMDs to share their experiences and the effects of these diseases on their daily lives. Participants from various countries across Europe are encouraged to take part.
The survey seeks to gather detailed information on how RMDs impact individuals' lives, focusing on their physical, emotional, and social well-being. The collected data will help researchers and health care providers understand the challenges faced by patients and develop better care strategies.
Key takeaways
Participation in this survey is crucial for improving the understanding and management of RMDs. The insights gained from patients will contribute to more effective treatments and support systems. EULAR encourages all patients with RMDs to participate and share their experiences to help advance care and research.
Click here to learn more about or take the survey.
EULAR Calls for Action to Tackle Rheumatic and Musculoskeletal Diseases
Background
EULAR has launched a new manifesto for 2024-2029, urging the European Union and national governments to take significant steps in addressing rheumatic and musculoskeletal diseases (RMDs). These diseases affect millions of people across Europe, causing pain, disability, and impacting their quality of life.
EULAR's manifesto highlights the urgent need for comprehensive strategies to manage RMDs. The focus is on improving prevention, early diagnosis, treatment, and rehabilitation. EULAR also stresses the importance of prioritizing RMDs within the EU's 'Healthier Together – NCD Initiative' and addressing the chronic shortage of rheumatologists and specialized health care professionals.
The manifesto has gained support from multiple Members of the European Parliament (MEPs) who recognize the challenges posed by RMDs. EULAR calls for integrated approaches that encompass health-related quality of life, education, and employment. The aim is to create inclusive and flexible environments for people living with RMDs, recognizing these conditions as a leading cause of disability.
The strategies proposed include promoting inclusive education and workplaces, increasing funding for research, and improving standards of care by addressing the shortage of specialized health care professionals.
Key takeaways
The EULAR 2024-2029 manifesto calls for urgent action from the EU and national governments to develop and implement comprehensive RMD strategies. By focusing on prevention, early diagnosis, and better care, the goal is to improve the quality of life for people with RMDs and reduce the overall burden of these diseases on society.
Promoting cooperation in inflammatory arthritis
Title of the study: Improving cross-sectoral care for patients with inflammatory arthritis: results from a first seminar with cross-sectoral involvement.
Background
There is a need to improve cross-sectoral care for people with inflammatory arthritis. The Danish Centre for Expertise in Rheumatology (CeViG) at the Danish Hospital for Rheumatic Diseases in Sønderborg, Denmark, is focussing on how to share knowledge with people involved in the care and management of inflammatory arthritis. Researchers from CeViG presented new survey data at the 2024 EULAR congress that highlight the benefits of cooperation between different stakeholders.
Study details
The study focused on inflammatory arthritis, which including diseases like rheumatoid arthritis, psoriatic arthritis, juvenile idiopathic arthritis, and ankylosing spondylitis. The survey data were collected from various stakeholders involved in the care of people with these conditions. The aim was to assess the benefits of cross-sectoral cooperation.
Cross-sectoral cooperation in healthcare means that different parts of the system – like public services, private companies, and non-profit organizations – work together to tackle health problems. This type of teamwork is crucial for people with inflammatory arthritis because it allows for a unified approach that brings together various healthcare and support services. By sharing expertise and resources, this cooperation can lead to new treatments and better-coordinated care, improving the overall quality of life for patients with this chronic condition.
To explore and facilitate cross sectoral collaboration, a 1-day seminar was held to bring together a group of 53 stakeholders with different backgrounds and interests, including multidisciplinary health care professionals and general practitioners, municipal representatives, politicians, public leaders, and patient research partners.
Findings
The survey showed that cooperation between different stakeholders improves the management of inflammatory arthritis. This cooperation helps in sharing knowledge and providing better care for patients, leading to improved outcomes.
Key takeaways
Improving cooperation between different sectors involved in the care of inflammatory arthritis patients is crucial. This approach enhances knowledge sharing and improves patient care. Further efforts should be made to foster such collaborations.
Click here to learn more about the study.
Implementing physical activity recommendations: Identifying key barriers and facilitators
Title of the study: Systematic review on barriers and facilitators for people with rheumatic and musculoskeletal diseases for adherence to EULAR physical activity recommendations
Background
EULAR – The European Alliance of Associations for Rheumatology – has recommendations aimed at promoting health-enhancing physical activity. Despite the established benefits and evidence supporting the efficacy of physical activity and exercise interventions in enhancing overall fitness, alleviating symptoms, improving quality of life, and positively impacting cardio health, there are challenges and a general gap between research findings and their implementation in real-world clinical settings. An abstract session at the EULAR congress focused on implementing physical activity recommendations in arthritis and addressing the challenges for patients to use them in their daily lives.
Study details
- Researchers reviewed existing research studies examining factors affecting adherence to EULAR’s physical activity recommendations.
- Across 68 selected articles, 29 different themes were identified – 9 of which were social, 16 environmental, and 4 systemic.
- The five most frequently found themes were having supportive family and friends, a supportive health professional, followed by costs, and access or proximity to adapted and supervised programs.
Findings
The session identified key factors to implementing physical activity recommendations. The discussions highlighted the gap between research findings and real-world application, emphasizing the need for strategies to bridge this gap.
Key takeaways
Addressing the barriers and promoting the facilitators to physical activity identified in the session could enhance the practical implementation of physical activity recommendations, ultimately improving outcomes for people living with arthritis.
Click here to learn more about the study.
Happy Holidays from the Global RA Network
December 20, 2023

Rheumatoid arthritis involves a disease process (like cancer or diabetes) where the body's immune system mistakenly attacks its own healthy joints. It is a relatively common disease-approximately 1 in 100 people get it-and is often devastating to a person's body if not treated properly. Within ten years of the onset of the disease, up to 50% of people living with RA are work disabled if untreated. For those living with RA, related inflammation in the arteries result in an increased risk of mortality. When moderate to severe, the disease reduces a person's life span by as much as a dozen years. Today, effective RA treatments exist, which can change these outcomes.
If you are a loved one, friend, co-worker of a person with RA, you likely have been struck by a range of traits and characteristics that reflect their resilience and adaptation to the disease. People living with RA are some of the most resilient, perseverant, patient, and compassionate people you will ever meet.
Those qualities are reflected by the member organizations of the GRAN who together, through collaboration, develop, test, and deliver solutions to address the unmet needs of RA patients in Europe and the Americas.
This holiday season, the Global RA Network is looking back at another year of significant achievements that had a positive impact on RA patient lives. We are also looking ahead to work in 2024 that will help advance RA treatment and care in Global RA Network member countries in Europe and the Americas.
In 2023, the Global RA Network’s advocacy efforts focused on advancing public awareness and government outreach to educate the public, media, and elected officials on issues of importance to the global RA community and push for policies favorable to RA care and treatment.
Looking ahead to 2024, the Global RA Network is focussing on learning about the lived experiences of RA patients accessing care in Europe and the Americas. This work will significantly contribute to a better understanding of current RA care models and the identification of emerging public policy priorities. The GRAN will share this valuable data with healthcare providers and policymakers to help improve RA care models, arthritis health policies, and overall patient outcomes.
To all our brothers and sisters living with RA around the world, we wish you a safe and healthy holiday season. We hope you will come back to visit us in the coming months and learn more about how you can help support our activities to dramatically change the lives of people living with RA in your country.
Together, we can jointly amplify the RA patient voice and advance RA treatment and care in Global RA Network member countries in Europe and the Americas.
ACE Reporting on American College of Rheumatology's 2023 annual scientific meeting - Important research news for Canadians living with arthritis
November 22, 2023
 Our Secretariat delegates from ACE attended the ACR Convergence meeting in San Diego, California from November 10 to 15, 2023. They have returned with valuable insights and the latest advancements in rheumatoid arthritis (RA) research. The annual scientific gathering, hosted by the American College of Rheumatology, offered hundreds of sessions about the latest research, advancements, and breakthroughs in arthritis to educate arthritis patients and professionals in every segment of rheumatology including clinicians, researchers, academicians, practice managers, pediatric rheumatologists, fellows in training, advance practice nurses, physician assistants, physical or occupational therapists from around the world. The meeting provided participants with access to in-person sessions, as well as on-demand recordings of each lecture and the 10-minute Q&A that followed most lectures, which were available to those joining remotely.
Our Secretariat delegates from ACE attended the ACR Convergence meeting in San Diego, California from November 10 to 15, 2023. They have returned with valuable insights and the latest advancements in rheumatoid arthritis (RA) research. The annual scientific gathering, hosted by the American College of Rheumatology, offered hundreds of sessions about the latest research, advancements, and breakthroughs in arthritis to educate arthritis patients and professionals in every segment of rheumatology including clinicians, researchers, academicians, practice managers, pediatric rheumatologists, fellows in training, advance practice nurses, physician assistants, physical or occupational therapists from around the world. The meeting provided participants with access to in-person sessions, as well as on-demand recordings of each lecture and the 10-minute Q&A that followed most lectures, which were available to those joining remotely.
Like last year’s conference, the inclusion of the Patient Perspectives Program allowed patients affected by rheumatic diseases, along with sponsoring organizations such as patient groups to share their personal stories with thousands of rheumatology healthcare providers, worldwide.
Now, let's delve into the key takeaways and updates that emerged from the forefront of RA research at this year's ACR Convergence meeting. For more content, please visit the ACR Convergence website.
Global Summit Addresses Need to Ensure Global Access to Essential Medicines
At a special session called the ACR Global Summit, Dr. Jayasree K. Iyer, CEO of the Access to Medicine Foundation, highlighted that despite advancements in drug development, nearly 2 billion people lack regular access to essential medicines, impacting health and increasing mortality. The focus on medicine access tends to prioritize diseases causing death, leaving chronic diseases like inflammatory arthritis, neglected.
The Foundation's research identified four key issues - availability, affordability, accessibility, and acceptability - that contribute to this gap. Dr. Iyer emphasized the importance of increasing the use of generic medicines and biologics and creating more equitable pricing strategies to improve access. She urged pharmaceutical companies to register products in developing countries and called for collective efforts in the healthcare community to ensure global access to medicines.
Rheumatic Disease in Indigenous Populations: North American Perspective
Dr. Cheryl Barnabe is a Métis rheumatologist and a Canada Research Chair in Rheumatoid Arthritis and Autoimmune Diseases. She is a Professor in the Departments of Medicine and Community Health Sciences, Cumming School of Medicine, University of Calgary. She is a Vice-Chair in the Department of Medicine (Indigenous Health), and the Deputy Director for the McCaig Institute for Bone and Joint Health.
In a special session on Rheumatic Disease in Indigenous Populations, Dr. Barnabe was one of three panelists who looked at the higher prevalence of arthritis in Indigenous populations, spoke about the reasons for this disproportionate rate of arthritis, and identified ways to deal with the gaps in models of care.
In her presentation, Dr. Barnabe focussed on the impact of arthritis on Indigenous Peoples in North America, including First Nations, Metis, Inuit, American Indian, Alaska Native, and Native Hawaiian communities. These groups, constituting about 5% of Canada's population and 2% of the United States’s population, are shown to have a higher prevalence of rheumatic diseases compared to the general population.
Dr. Barnabe’s research described the significant challenges faced by Indigenous Peoples, such as lower chances of recovering from these diseases, increased reliance on health services, and unique circumstances where social relationships and community roles play a crucial role. She also spoke about the various factors affecting healthcare access, such as racism, economic status, geographical distance, and difficulties in navigating the healthcare system. Additionally, Dr. Barnabe’s research raised issues surrounding medication access including trust concerns, stigma related to medication use, challenges in the supply chain, and financial burdens associated with reimbursement coverage for arthritis medications.
In her study, Dr. Barnabe proposes practical solutions to address these health disparities. First, she suggests improving the relationship between patients and healthcare providers by adopting trauma-informed care. This approach aims to create a safer and more supportive environment for individuals who have experienced trauma. Another key recommendation is enhancing access and coordination through navigation models, making it easier for Indigenous individuals living with arthritis to navigate the complex healthcare systems in North America. Dr. Barnabe also emphasizes the importance of expanding treatment options to reduce the burden on patients and support informed decision-making.
Dr. Barnabe concluded her presentation by describing the significance of collaboration among family, community, primary care, and other support systems. By fostering a holistic approach to healthcare, Indigenous communities can better address the challenges posed by arthritis. She called for policy changes, emphasizing the need for better medication access and restructuring health systems to ensure fair and effective care for Indigenous Peoples living with arthritis.
Special Lecture Proposes Shift in RA Therapy from Weakening the Immune System to Strengthening It
Researchers exploring rheumatoid arthritis (RA) have uncovered that the immune systems of patients with RA face a breakdown in self-tolerance, leading to persistent inflammation. What is behind these processes has been challenging to identify. Dr. Cornelia M. Weyand, MD, PhD, Professor of Medicine and Immunology at the Mayo Clinic College of Medicine and Science and Professor Emerita of Medicine, Stanford University School of Medicine, addressed these challenges when she delivered the Klemperer Memorial Lecture, titled “Rheumatoid Arthritis as a Mitochondrial Disease” at the ACR annual scientific meeting.
Dr. Weyand described that in patients with RA, the immune system is under a kind of stress related to how cells generate energy. Malfunctions in the mitochondria, the cell's powerhouses, play a crucial role. Mitochondria are essential components of nearly all cells in the body, providing energy to carry out biochemical reactions and other cellular processes. Mitochondria make energy for cells from the chemical energy stored in the food we eat.
Inflammation in RA patients occurs when aged T-cells accumulate and cause inflammation, giving rise to inflammatory cells with high tissue invasiveness. Mitochondrial defects in this inflammation process result in energy depletion and miscommunication with other cell components. According to Dr. Weyand, these mitochondrial defects trigger the excessive production of tumor necrosis factor (TNF) alpha, a key feature of inflammation in RA. Traditionally, RA therapy involved suppressing the immune system to reduce inflammation, but Dr. Weyand challenges this approach. She believes that immunosuppressive medications make patients vulnerable, as observed during the COVID-19 pandemic. Dr. Weyand advocates for a shift toward repairing and strengthening the immune system rather than suppressing it: “During the COVID-19 pandemic, it became clear that the anti-inflammatory and immunosuppressive medications we give our patients make them immunocompromised. Immunology has taken a new direction, and the next horizon we are moving toward with RA is not to continue suppressing the immune system but repairing and strengthening it.”
This new direction in understanding and treating RA could lead to new ways to enhance the immune system's function, providing hope for more effective and tailored therapies in the future.
What Role Does Poor Sleep Play in Pain Experienced by RA Patients?
ACR Convergence Abstract: Sleep Disturbance Predicts Pain Interference in Patients with Early Rheumatoid Arthritis in a Prospective Real-World Cohort
A study led by a large number of leading Canadian experts focused on patients with early rheumatoid arthritis (RA) who, despite taking strong medications, often experience persistent pain that isn’t easily explained by clinical measures or experience. Sleep disturbances are common in RA patients and may impact how they perceive pain. While previous research showed a link between one night of poor sleep and increased pain the next day, this study aimed to understand if early sleep disturbances influence long-term pain outcomes.
The study used data from the Canadian Early Arthritis Cohort, involving 502 patients with early RA. Participants reported their sleep quality and pain interference using PROMIS measures over 24 months. The results showed a significant association between sleep disturbances and pain interference. Better sleep six months prior was linked to less pain interference at the subsequent evaluation.
These findings highlight the importance of addressing sleep issues in managing pain for early RA patients. Early identification and intervention for sleep disturbances could potentially improve long-term pain outcomes. The study underscores the need for further research to explore underlying mechanisms and potential interventions targeting sleep to alleviate pain in RA.
Hydroxychloroquine Lowers Risk of Non-alcoholic Fatty Liver Disease in RA Patients
ACR Convergence Abstract: Hydroxychloroquine Is Associated with a Decreased Risk of Non-alcoholic Fatty Liver Disease in Patients with Rheumatoid Arthritis: A Population-based, Cohort Study
The latest research presented at ACR Convergence 2023 suggests that treating rheumatoid arthritis (RA) with hydroxychloroquine (HCQ) may reduce the risk of non-alcoholic fatty liver disease (NAFLD), especially in women and men under 50 years old. RA is an autoimmune inflammatory disease affecting joints and other organs, and NAFLD is a prevalent condition in RA patients.
Drawing on data from Taiwan's National Health Insurance Research Database (2000-2020), the study included over 21,000 patients. The results indicate that 399 patients (1.86%) developed NAFLD after eight years, and taking HCQ was associated with a significantly lower risk of NAFLD, particularly in women under 50. The potential explanation lies in HCQ's impact on adiponectin, a factor linked to insulin resistance, inflammation, and NAFLD. The study revealed common NAFLD risk factors like obesity, higher prednisone doses, and nonsteroidal anti-inflammatory drugs (NSAIDs). However, conventional risk factors such as diabetes and high cholesterol were not prevalent in this sample of RA patients.
Despite the study's limitations using claims data, the findings highlight a potential benefit of HCQ in reducing NAFLD risk for RA patients. Nevertheless, the researcher, Hsin-Hua Chen, emphasizes the need for double-blind randomized controlled trials to confirm HCQ's preventive or therapeutic effect on NAFLD. Until then, regular liver function tests are recommended every three months for all RA patients and monthly for those taking medications with potential liver toxicity. This research adds valuable insights to managing RA and associated conditions, promoting better care for individuals with RA.
Canadian Researchers Show AI Model Accurately Identifies, Predicts Joint Damage in Hand X-Rays
Artificial intelligence in health care is a key topic at this year’s ACR annual meeting. Researchers presented a deep learning system that accurately identifies and predicts joint space narrowing and erosions in hand X-rays of patients with rheumatoid arthritis (RA). Deep learning is a type of machine learning and artificial intelligence (AI) that imitates the way humans gain certain types of knowledge. Deep learning models can be taught to perform classification tasks and recognize patterns in photos, text, audio, and other various data. Traditional methods of evaluating RA can be time-consuming and require specific expertise.
The study, led by Dr. Carol Hitchon, from the University of Manitoba, explores the potential of machine learning to enhance RA detection and diagnosis. Using a neural network (CNN) called You Only Look Once (YOLO), the researchers trained the model to detect joints in hand radiographs. YOLO is known for its real-time object detection capabilities and efficiency in image processing. The model developed by Dr. Hitchon’s team achieved high accuracy in identifying target joints.
The researchers also use a deep learning and AI model to provide highly accurate predictions for joint space narrowing and erosion.
Despite the promising results, the study acknowledges limitations, such as a sample of patients primarily composed of white women. The findings may not be universally applicable, and the researchers emphasize the need for replication in diverse groups. Additionally, the model currently lacks continual learning ability, but the team is working on a new deep-learning framework to address this limitation.
Dr. Hitchon underscores that while AI models cannot replace human radiologists, they serve as excellent complementary tools, enhancing the overall quality and efficiency of radiograph scoring analysis. The study envisions these models being applied to interpret large volumes of X-rays in clinical trials, showcasing the potential for AI to assist and complement human expertise in the field of rheumatology.
Biomarker-Driven Trials Have the Potential to Usher in a Personalized Approach to RA Treatment
At a session on Precision Clinical Trial Design in Rheumatoid Arthritis, Dr. Costantino Pitzalis, MD, PhD, Versus Arthritis Professor of Rheumatology, Queen Mary University of London, discussed how the way we conduct clinical trials for rheumatoid arthritis (RA) needs a more personalized approach. He emphasized the need to move away from a one-size-fits-all method and select patients based on their likelihood of responding to treatment. While current trials have led to effective RA therapies, there are still unmet needs, with some patients not responding well to existing treatments.
Dr. Pitzalis's research focuses on finding predictive molecular biomarkers for treatment response. Traditional blood biomarkers have not been successful, so his group studied synovial fluid using ultrasound-guided synovial biopsies. They identified three disease types based on genetic signatures that respond differently to RA therapies.
This work has led to two biomarker-driven clinical trials under the 3TR project. The first, 3TR PARTNER-RA, explores the response to abatacept in early RA, and the second, 3TR Precis-The-RA, investigates the response to sarilumab and etanercept. Dr. Pitzalis hopes these trials will show the usefulness of synovial biopsies, potentially integrating them into routine care for higher response rates.
He acknowledges the challenges of the journey toward precision medicine but is optimistic that these trials can help identify the right treatment for each patient from the start.
Watch Nenad Nedic from patient association ORS in Serbia talk about the RA Dashboard for his country!
October 26, 2023
Rheumatoid Arthritis (RA) is a prevalent disease that affects approximately 30 million people around the world. However, the models of care for this disease differ from country to country, and even within countries, there exist inequalities. To address this issue, a year ago, we launched a tool called the RA dashboard.
This tool helps to depict the portrait of rheumatoid arthritis and the gaps in the delivery of models of RA care in member countries of the Network in Europe and the Americas. RA dashboards are currently available for 13 countries and can be accessed on the Global RA Network’s website. The data presented in the Dashboard has been researched and collected by member associations and the Network's secretariat using local publicly available literature, existing open data sets of government agencies and research organizations, and results from the Global RA Network international survey on models of RA care.
In a filmed interview with Isabelle Troïtzky from the Network secretariat, Nenad Nedic, an activist and volunteer at Udruženje obolelih od reumatskih bolesti Republike Srbije, the Organization for patients with rheumatic disease of Serbia (ORS), talks about the RA dashboard for his country. He explains the work of his organization and how ORS used the dashboard to advocate for a better model of care for RA patients so their quality of life can improve.
Watch the interview here.
Access other interviews about the RA dashboard with leaders from ACE (Canada), NRAS (UK) and AFLAR (France) and compare data from the different country RA dashboards by clicking here.
The Global RA Network collaborates with Pfizer to launch a new video to spread awareness about RA on World Arthritis Day
October 12, 2023
October 12 is observed as World Arthritis Day (WAD) every year. To mark this day, the Global RA Network has teamed up with Pfizer to create an informative video on rheumatoid arthritis (RA). The video aims to create awareness about RA and its impact on people living with it around the world. The video is being shared widely on social media platforms of member organizations of the Global RA Network. We urge you to watch the video and help us spread the word by sharing it with your networks.
The arthritis community worldwide comes together on this day to educate and inform the public about various aspects of arthritis and its impact on people living with it. The community also advocates for better models of care where patients can see their rheumatologist as frequently as recommended by the guidelines and don't have to wait longer than three months for their first appointment.
Arthritis is a condition that comes in many forms, with rheumatoid arthritis (RA) being one of them. RA is a major cause of disability and affects approximately 30 million people worldwide. If left untreated, up to 50% of people with RA become work disabled within ten years of the onset of the disease. RA is also linked to a number of other health problems, such as a higher risk of heart attacks and strokes, depression, osteoporosis, fractures, and even some cancers, especially lung and lymphoma. The disease creates a significant burden on health systems, resulting in direct healthcare costs, as well as indirect costs from lost employment, sick leave, and absenteeism.
Although RA can be difficult to recognize, an early diagnosis is essential for effective disease management. Understanding the disease can also empower patients and help their loved ones, employers, and acquaintances to better comprehend the challenges they face daily and support them as needed.
Awareness tools like this new video are crucial to improving people's understanding of rheumatoid arthritis. Our gratitude goes to Pfizer for this incredible initiative and for collaborating with patients through our international network of patient organizations to make it possible.
Our member organizations work tirelessly to increase education and enhance the lives of arthritis patients. On this World Arthritis Day, and throughout the year, we encourage everyone to check out their social media posts and visit their websites to explore the fantastic resources they offer.
Let's unite for a world where rheumatoid arthritis is more comprehensively understood, and models of care are optimal!
Members of the Global RA Network share their key initiatives for rheumatoid arthritis patients at a workshop organized during EULAR 2023
July 5, 2023

The 2023 EULAR Congress in Milan early June was a fantastic opportunity for the members of the Global RA Network to meet in person but also virtually over a very productive annual workshop. We exchanged a wide range of ideas and experiences and took time to discuss how we could address RA and health inequities as a network of patient organizations.
The first part of our workshop was devoted to sharing the main initiatives that our member organizations have carried out in 2023 in their respective countries to address one of the Network's priorities. They did so by means of poster summaries, highlighting the context, target audiences, activities, results and next steps of their projects. All the projects were highly innovative and successful. They all contributed greatly to improving awareness, education and quality of life for rheumatoid arthritis patients. Below you'll find a sample of these initiatives, with a quick summary for each, and a link to the more detailed posters.
Take a look, get inspired and get involved!
Arthritis Consumer Experts (ACE) in Canada conducted a national Survey on Health Inequities in Arthritis Care to raise awareness of the disparities in access to arthritis care in Canada between White people and Black, Indigenous people and people of colour (BIPOC) living with arthritis. The Survey was promoted through social media and supported by a series of webinars on Indigenous health. In a second phase, meetings are planned with provincial and territorial health ministries to present the Survey results, the state of arthritis care for BIPOC people, and the Canadian RA Dashboard.
The French League Against Rheumatism (AFLAR) has developed an information and education video series (3 videos) about RA including patient testimonials, the creation of a panel of patients, working groups on pain with patients, a rheumatologist, an expert in therapeutic patient education, a community pharmacist and consultation with the Minister of Health on biosimilar medicines.
The Italian National Association of People with Rheumatological and Rare Diseases (APMARR) created the “Buono da mangiare” (Good to eat) program promoting the benefits of eating well – nutrition (good and right food intake), socialization (increased conviviality) and pleasure (savory meals, taking the time to eat), taking care of oneself for a good quality of life – with RA patients, care givers and doctors. It started with a survey about nutrition and produced a book of recipes developed together with Italian scientific society of nutrition and a team of rheumatologists, videos and an application. The book and program got a well-deserved award.
Arthritis Ireland launched a Clinic Referral Program whereby hospital clinics refer newly diagnosed patients to Arthritis Ireland who in turn offer support to them to empower them and help them effectively self-manage their disease. The program is growing with an increased number of referrals and positive feedback as it allows patients to receive personalized information and creates one-on-one relationships, contributing to better care.
The National Rheumatoid Arthritis Society (NRAS) in the United Kingdom surveyed participants in SMILE-RA (Self-management Individualised Learning Environment in Rheumatoid Arthritis), an e-learning program created by NRAS and providing innovative, evidence-based, high quality educational content which is accessible to individuals and their families and carers for free, 24/7. The survey results demonstrate that the program improves the patients’ understanding of the importance of supported self-management, as well as many of the components of patient empowerment. NRAS promoted it through a large marketing campaign, on its social media channels, and by encouraging health care professionals to share about it. Over 2,000 people have participated in SMILE-RA to date and health care professionals agree that the program is a great learning resource.
The Association of patients with rheumatic diseases of the Republic of Serbia (ORS) has implemented its "Expert Patient Program”, which involves training its members - patient activists - to become expert patients and organizing workshops with medical students. At these workshops, participants are introduced to the Serbian RA dashboard and reminded of the importance of collecting data.
The Rheumatoid Arthritis Liga (RA Liga) in Belgium organized a traveling art exhibition entitled "ART and RA, hand in hand" and toured it to raise awareness of RA and early diagnosis in a creative way, with the patients' message behind the artwork, in collaboration with hospitals and rheumatologists. RA Liga promoted it via local government, artists, several associations, caregivers, and local publicity.
Congratulations to our member organizations across Europe and the Americas for their energy, creativity and dedication.
Please contact us at secretariat@globalranetwork.org or the members of the Global RA Network (see the homepage for contact information) with any questions you may have on their initiatives.
EULAR 2023 Highlights
June 27, 2023

The EULAR congress of rheumatology was held live in the vibrant city of Milan from May 31st to June 3rd, 2023. The event once again boasted a diverse and informative program that left attendees feeling inspired and educated.
During the congress, the secretariat of the Global RA Network was present alongside numerous member organizations. We took advantage of this opportunity to host a workshop for our members, which was met with great success! Each organization presented a major initiative they had undertaken in 2023 that significantly contributed to improving the patient journey for those with RA, or advocated on their behalf to various stakeholders. All of the initiatives were innovative and strongly aligned with the Network's priorities. As a group, we discussed the health disparities associated with RA in our respective countries and how we can work together, as well as individually, to address these challenges. The discussion generated interesting ideas, some of which will be implemented in the coming year. Stay tuned!
The members of the Global RA Network also played an active role in the EULAR congress, presenting research, hosting conferences, and managing booths. Here are just a few examples of the presentations:
- Slađana Rumpl Tunjić from Association Remisija (Croatia) and EULAR Young PARE chaired the session entitled 0 – 100 in 75 minutes; RMDs have no age
- Tanita-Christina Wilhelmer from Österreichischen Rheumaliga/Jung und Rheuma (Austria) gave a presentation about The use of objects to experience inflammatory rheumatic diseases in order to increase knowledge and understanding through perspective-taking, with a focus on enhancing empathy
- Suncica Djordjevic from ORS-Udruženje obolelih od reumatskih bolesti Republike Srbije (Serbia) held a poster tour
- At the session entitled The Clinic as a Classroom – teaching and learning with patients, Nenad Nedić from ORS (Serbia) presented the case study Serbia: Patient Expert implementation in Serbia following KTP and Andri Phoka from the Cyprus League Against Rheumatism (Cyprus) and AGORA presented case study Cyprus: Patient Expert implementation in Cyprus following KTP.
- Ellen Wang from Arthritis Consumer Experts (ACE) presented in the session entitled The promise of health literacy in clinical care.
Our team has put together a collection of noteworthy research and news related to rheumatoid arthritis that was discussed at EULAR. We have provided a summary of this information below. If you require additional information, the conference content is accessible online on-demand until December 31, 2023.
Summary of significant research related to rheumatoid arthritis
Cancer Risk in Rheumatoid Arthritis Patients Not Due to Medications
Rheumatoid Arthritis (RA) affects 24.5 million people worldwide and has been associated with increased cancer risks.
Researchers at EULAR looked at whether the increased cancer risk in RA patients is due to the disease itself or the medications used for treatment.1 The researchers compared cancer rates in RA patients receiving different types of treatments with those in the general population.
The results showed that RA patients had a higher overall cancer risk compared to the general population, regardless of the medications they were taking. This suggests that the increased cancer risk is not due to the drugs used to treat RA. Instead, it may be related to the underlying inflammation and immune system abnormalities associated with the disease.
This finding is important because it helps researchers and clinicians better understand the potential risks associated with RA and its treatment. It also reassures patients that their medications are not increasing their cancer risk. The study highlights the need for further research to explore the relationship between RA and cancer and to develop strategies to reduce this risk in RA patients.
Impact of Obesity on Rheumatoid Arthritis Treatment Outcomes
A study was presented that explored how obesity affects treatment outcomes in RA patients.2 Researchers analyzed data from over 1,500 RA patients, comparing the effectiveness of various treatments between patients with obesity and those without.
The results showed that obese RA patients had a lower likelihood of achieving remission (a state where the disease becomes inactive) and experienced a slower improvement in their symptoms compared to non-obese patients. This suggests that obesity can negatively impact the effectiveness of RA treatments.
These findings are crucial for both patients and healthcare providers as they highlight the importance of addressing obesity in the management of RA. By focusing on weight loss and maintaining a healthy weight, RA patients may improve their chances of successful treatment outcomes. This study also emphasizes the need for further research to explore the underlying mechanisms that link obesity and RA treatment response and to develop targeted strategies to enhance treatment effectiveness in obese RA patients.
Biosimilar Biologics as Effective as Originator Biologics for Rheumatoid Arthritis Treatment
A systematic review and meta-analysis published in JAMA Network Open compared the effectiveness and safety of biosimilar drugs to their biologic originator counterparts in treating RA.3 Biosimilars are biological medications that are highly similar to biologic originator medications, offering a potentially more affordable treatment option for RA patients.
The researchers analyzed data from multiple clinical trials involving over 3,000 RA patients treated with either biosimilars or originator biologics. The results showed that biosimilars were just as effective in reducing RA symptoms and had similar safety profiles as the originator biologic medications.
This finding is significant for RA patients and healthcare providers, as it demonstrates that biosimilars can be a viable and cost-effective alternative to expensive biologic originator medications without compromising treatment outcomes. The study also supports the ongoing adoption and use of biosimilars in the management of RA, potentially increasing access to effective treatments for more patients.
Maternal Rheumatoid Arthritis and Autism Risk in Offspring
A study from Sweden presented at EULAR examined the potential link between maternal rheumatoid arthritis (RA) and the risk of autism spectrum disorder (ASD) in their children.4 Researchers analyzed data from more than 1.5 million children, including those born to mothers with RA and those without the disease.
The results indicated that children born to mothers with RA had a slightly increased risk of developing ASD compared to children born to mothers without RA. This suggests that maternal RA may be a contributing factor in the development of ASD in offspring.
This research is important for expectant mothers with RA and healthcare providers, as it highlights the need for increased awareness and monitoring of ASD risk in children born to mothers with the disease. It also emphasizes the importance of further studies to better understand the relationship between maternal RA and ASD, as well as potential interventions to reduce this risk.
High Mortality Rates Linked to Depression in Rheumatoid Arthritis Patients
Anxiety and depression are the mental health issues most commonly associated with RA, and it is well-established that there is a link between mental health issues and poor health outcomes.
A Danish abstract presented at EULAR explored the relationship between depression and mortality rates in patients with RA.5 Researchers analyzed data from over 2,000 RA patients, including those with and without depression, to determine whether depression could be associated with higher mortality rates in this population.
The results revealed that RA patients with depression had a significantly higher mortality rate compared to those without depression. This suggests that depression may be an important factor contributing to the increased risk of death among RA patients.
These findings are crucial for RA patients and healthcare providers, as they emphasize the importance of addressing mental health issues like depression in the comprehensive management of RA. Early detection and treatment of depression in RA patients may not only improve their psychological well-being but also potentially reduce the risk of premature death.
The study highlights the need for further research to better understand the underlying mechanisms linking depression and mortality in RA patients, as well as the development of targeted interventions to improve mental health outcomes in this population.
Artificial Intelligence Enhancing Rheumatoid Arthritis Patient Care
At the congress, several studies were presented that explored the potential of artificial intelligence (AI) to improve patient care and management for individuals with RA. Researchers developed AI-based tools designed to assist healthcare providers in making better treatment decisions, monitoring disease progression, and predicting patient outcomes.
A Japanese team of researchers looked at the use of machine learning in predicting the development from undifferentiated arthritis to RA.6 Undifferentiated arthritis (UA) is arthritis that does not fit a specific diagnosis. Half of the UA undergo spontaneous remission, while 30% of cases develop RA. In UA, identifying patients at high risk for developing RA and providing close monitoring for those patients is required for early diagnosis and treatment.
The researchers concluded that applying a machine learning approach might enable identifying patients at high risk of RA progression and improve the clinical management of undifferentiated arthritis patients.
This study highlights the growing importance of incorporating advanced technology like AI into healthcare, as it offers the potential to improve both patient care and healthcare provider efficiency. Further research is now needed to refine AI algorithms and evaluate their long-term effectiveness in managing RA.
Comparing Human and Computer Accuracy in Predicting Rheumatoid Arthritis Progression Using MRI
Predicting early RA from MRI images of the hands and feet can help people access timely treatment, which may possibly change the disease course. Traditionally this is done by radiologists and rheumatologists using a scoring sheet to manually identify key features from the MRI scans.
An abstract presented by researchers from Leiden University Medical Center evaluated the accuracy of human specialists versus computer algorithms in predicting RA progression using magnetic resonance imaging (MRI).7 MRI is a crucial tool for assessing joint inflammation and damage in RA patients, helping healthcare providers make informed decisions about treatment plans.
Researchers compared the ability of experienced radiologists to predict RA progression using MRI with that of a computer algorithm specifically designed for this task. The study involved analyzing MRI scans from a large group of RA patients and determining how well both human experts and the computer algorithm could predict disease progression over time.
The results showed that the computer algorithm was more accurate in predicting RA progression than human specialists. This suggests that incorporating advanced technology like computer algorithms into RA management could potentially improve patient care by providing more precise and reliable predictions of disease progression.
T-Cells: The Missing Link in Pre-Clinical Rheumatoid Arthritis?
A study presented at the conference investigated the role of T-cells, a type of immune cell, in the early stages of RA development, specifically during the pre-clinical phase.8 Understanding the underlying mechanisms of RA onset is crucial for developing effective prevention and early intervention strategies.
Researchers analyzed blood samples from individuals at risk of developing RA and compared their T-cell profiles to those of healthy individuals. They aimed to identify specific T-cell patterns that could potentially serve as biomarkers for predicting the onset of RA.
The findings revealed significant differences in the T-cell profiles between individuals at risk of RA and healthy individuals. This suggests that T-cells might play a crucial role in the early development of RA, even before the onset of clinical symptoms.
These results are important for RA patients and healthcare providers, as they highlight the potential of T-cell profiling as a diagnostic tool for identifying individuals at risk of developing RA. Early detection and intervention could potentially prevent or delay the onset of clinical symptoms, improving long-term patient outcomes.
References
- Wang, F., “Large-scale real-world data analyses of cancer risks among patients with rheumatoid arthritis” International Journal of Cancer, May 2023 https://onlinelibrary.wiley.com/doi/abs/10.1002/ijc.34606
- Maglio, C., “Obesity is a risk factor for poor response to treatment in early rheumatoid arthritis - A NORD-STAR spin-off study” Annals of the Rheumatic Diseases, June 2023
- Ascef BDO et al., “Therapeutic Equivalence of Biosimilar and Reference Biologic Drugs in Rheumatoid Arthritis,” JAMA Network Open, June 2023
- Sandin, S., et al., Maternal rheumatoid arthritis and risk of autism in the offspring,” Cambridge University Press, April 2023
- Vestergaard SB, et al. Self-management behaviour, anxiety and depression in patients with inflammatory arthritis -a cross sectional nationwide study among >12,000 Danish patients. Presented at EULAR 2023; Abstract OP0176-HPR.EULAR01.06.2023Kilchberg, Switzerland
- Fujii, T., et al. “A Machine Learning Model that Predicts RA Progression from Undifferentiated Arthritis,” EULAR, June 2023.
- Li Y, et al. “Exploring the Use of Artificial Intelligence in Predicting Rheumatoid Arthritis, Based on Extremity MR Scans in Early Arthritis and Clinically Suspect Arthralgia patients.” EULAR, June 2023
- Anang, D., “Lymph nodes and peripheral blood harbor expanded t cell receptor clones during the preclinical phase of rheumatoid arthritis which persist on arthritis onset.” EULAR, June 2023.
AFLAR presents France’s RA Dashboard
May 16, 2023
The RA dashboard is worth some introductions! Françoise Alliot-Launois, the president of AFLAR, the French League Against Rheumatism, responds to Isabelle Troïtzky from the Global RA Network secretariat in a new interview on AFLAR and the important features of the French RA dashboard. Click here to view the video interview. The original video is in French, but captions (subtitles) are available by choosing the (cc) option at the bottom of the video screen on YouTube and selecting the language of your choice in the settings.
The Global RA Network and its members introduced the RA dashboard almost a year ago as a useful advocacy and education tool to help advance models of care for those with rheumatoid arthritis. Thirteen (13) countries in Europe and the Americas have already released a dashboard, and more are presently gathering key information on the disease and how RA care and treatment are provided in their nations to develop their own. Hovering over the current RA dashboards enables comparison of the RA situation across regions and examining them over time allows to observe its evolution. As new data become available, the RA dashboard will be updated to reflect this. So, make plans for more trips to the RA dashboard page!
#CRArthritis interviews at the CRA & AHPA Annual Scientific Meeting
March 8, 2023
Left to right: Ellen Wang, Cheryl Koehn, Kelly Lendvoy, Isabelle Troïtzky, Anita Chan
Isabelle Troïtzky, Global RA Network’s Secretariat, participated as an interviewer for the Arthritis Broadcast Network’s #CRArthritis event at the 2023 Canadian Rheumatology Association and Arthritis Health Professions Association Annual Scientific Meeting. There are over 40 and counting conversations with leading health care professionals, researchers and patient organizations on a range of arthritis-related topics. To view the interviews, please click on the links below:
Arthritis Broadcast Network is Canada’s largest patient-led arthritis news outlet and was co-founded and led by our Canadian member Arthritis Consumer Experts and Arthritis Research Canada. The platform provides a wealth of information, advice, and resources for patients and their families. Please bookmark this page for your reference: www.arthritisbroadcastnetwork.org
Inequities in Arthritis Care in Canada: The Black, Indigenous and Person of Colour (BIPOC) Experience
February 23, 2023
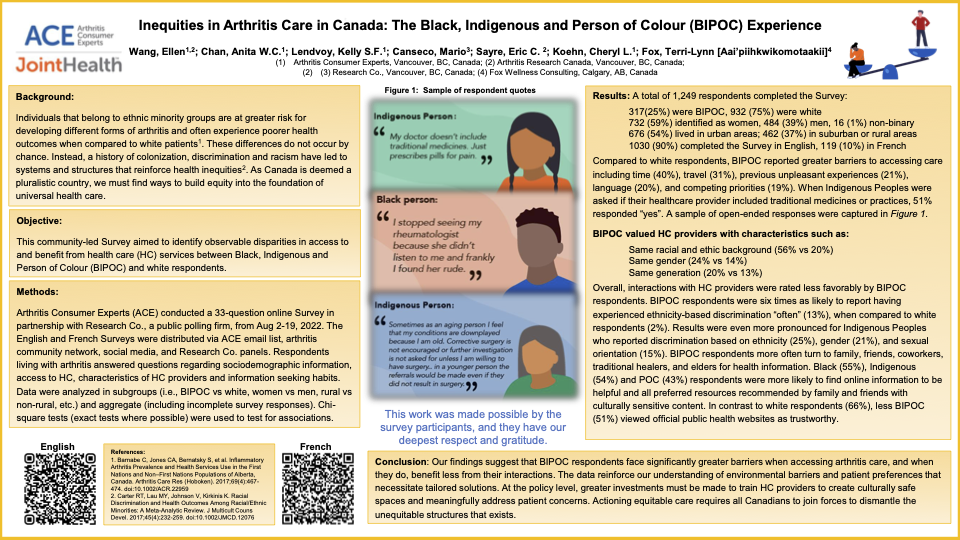
Our Canadian member, Arthritis Consumer Experts, took part in the 2023 Canadian Rheumatology Association and Arthritis Health Professions Association Annual Scientific Meeting in Quebec City from February 8-11, 2023. They attended informational sessions, interviewed and met with leading Canadian rheumatologists, researchers and representatives from other patient organizations. Further, Programs Coordinator, Ellen Wang, shared findings from their latest Survey on health inequities in arthritis care in Canada through a poster presentation. The poster was well received and was awarded Best Trainee Abstract.
Ellen is a MPT/PhD student under the supervision of Dr. Linda Li at the University of British Columbia. She received her Master and Bachelor of Science in Kinesiology at the University of Waterloo. She joined Arthritis Consumer Experts (ACE) at the end of 2021 and contributes to content development for JointHealthTM programs and the Arthritis Broadcast Network.
Ellen shared an important dialogue with attendees of the poster session by highlighting inequities in access to and benefit from health care services between Black, Indigenous, and person of colour (BIPOC) and white in Canada. The poster highlighted different aspects of the Survey: socioeconomic status, access to care (including traditional medicines and practices), interactions with health care providers (including primary care provider and rheumatologists), unfavourable experiences, and information seeking habits. To take a closer look at the poster, click here.
ACE’s Survey results suggest that BIPOC respondents face significantly greater barriers when accessing arthritis care, and when they do, benefit less from their interactions. They further reinforce current health literature that calls for training health care professionals to create safe spaces, meaningfully address patient concerns and ensure the delivery of equitable care.
The Survey included 33 questions and was conducted online in English and French from August 2 to August 19, 2022 with 1,249 respondents and in partnership with public polling firm Research Co. Survey analysis was conducted for three Survey groups: Black, Indigenous, and people of colour (BIPOC) respondents versus white respondents, rural respondents versus non-rural respondents, and women respondents versus men respondents versus non-binary respondents.
To find more details about the survey, please visit: https://bit.ly/JHIHealthInequitiesSurveyReportEN
NRAS and ACE RA Dashboard
February 16, 2023

In June of last year, as part of their initiatives to improve models of care for people with rheumatoid arthritis, the Global RA Network and its members launched a new powerful advocacy and education tool: the RA Dashboard.
Developed in collaboration with leaders from member RA patient organizations, the Dashboard presents key data about the disease and the delivery of RA care and treatment in Europe and the Americas.
Thirteen (13) countries have already published a dashboard. In two videos, our members from Canada and the UK – Arthritis Consumer Experts (ACE) and National Rheumatoid Arthritis Society (NRAS) - explain key highlights of the dashboard for their countries and share how they will be using it to advocate and educate others about RA. Watch their videos by clicking on the links below:
We will publish here and on Facebook and Twitter other similar interviews with members from other countries. We invite you to come back often!
ASOPAN's posters at last EULAR congress
January 4, 2023
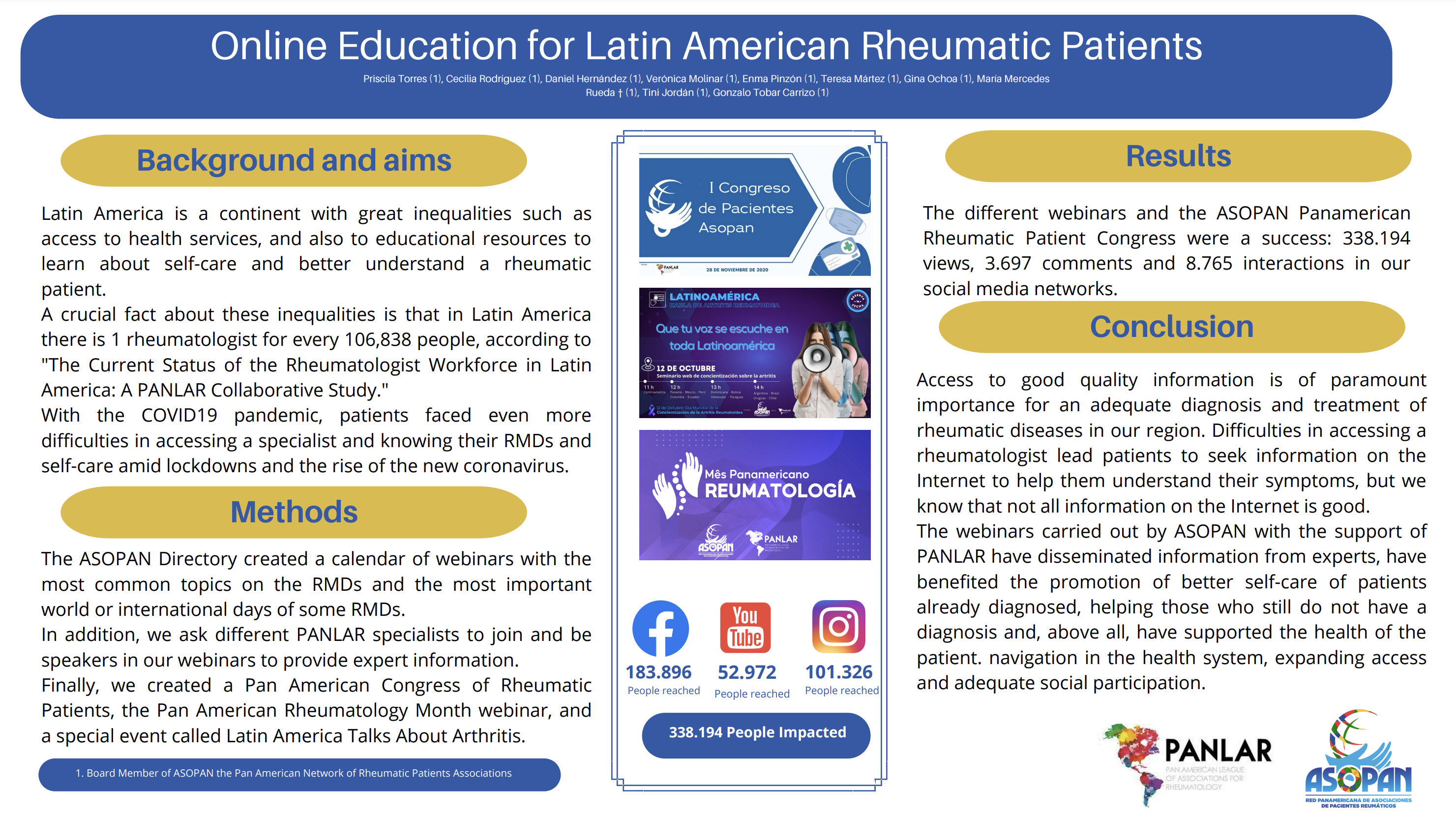
Last October in Copenhagen, ASOPAN, the pan-American network of arthritis patient associations, presented three posters about their programs in Latin America at the Best Practices Fair at EULAR PARE.
The first one introduces the Pan-American Manifesto for Rheumatic Diseases, a series of 12 recommendations about different aspects of care needs and difficulties that patients with rheumatic and musculoskeletal diseases (RMDs) face in the region: prevention, detection, timely diagnosis, comprehensive care by a multidisciplinary team in specialized centers, the role of patient organizations and their participation in health policies.
The second one describes the Expert Patient Program that promotes the formation of expert patient self-care teams in 3 countries of the region, which are able to help other patients to control their RMDs and their health in a global way, contributing to expanding quality and better management of RMDs. A pilot was launched, and the program will be expanded to other Latin American countries in the future.
The third poster presents the Online Education Program for Latin American Rheumatic Patients including webinars on the most common topics about RMDs and various events such as the Pan American Congress of Rheumatic Patients, the Pan American Rheumatology Month webinar, and a special event called Latin America Talks About Arthritis. This program helps patients access good quality information that is key to adequate diagnosis and treatment of rheumatic diseases on a continent that presents great inequalities as access to health services and educational resources are concerned.
Please click on the links below to access the posters.
ACR Key RA research takeaways - 2022
November 24, 2022

Our members attending this year’s ACR Convergence conference in Philadelphia brought back some interesting insights on RA research and discussions. The American College of Rheumatology’s annual scientific meeting took place from November 10 to 14 and gathered more than 9,000 in person and 4,300 virtual rheumatology professionals and patients from 104 countries. It included nearly 2,000 abstracts and expert presentations and hundreds of educational sessions for clinicians, researchers, academicians, practice managers, pediatric rheumatologists, fellows in training, advance practice nurses, physician assistants, physical or occupational therapists. This year, it also offered the Patient Perspectives Program whereby patients affected by rheumatic disease, along with a sponsoring organization such as a non-profit patient group, presented their stories.
Below are some interesting updates.
For more content, please visit the ACR Convergence website.
Patients Share the Stage at ACR
Attendees heard from Puja Khanna, MD, MPH, Associate Professor and Associate Chief of Clinical Affairs and Service Chief for Rheumatology at the University of Michigan who moderated the “Patient Perspectives” session and stated: “The patient perspective is more than a talking point in rheumatology, it’s a vital part of understanding and treating autoimmune disease.”
In this special session, attendees listened to two dozen patients who spoke about their personal experience of life with arthritis: their stories on everything from vaccinations during the COVID-19 pandemic, to the need to monitor one’s own medical records, to finding a new rheumatologist, and much more. The session, along with a two-hour virtual poster session, represented an unprecedented platform for the ACR to provide for the patient voice - an acknowledgement of the key role patients play in arthritis research, prevention, treatment and management.
At the presentations, speakers took the audience through the patient’s journey telling their personal stories about how they coped, revisited their goals and dreams, and the unforeseen gaps in their care. Their key message to the researchers and rheumatologists: When you are open to hearing the patient side, you can create that critical partnership that gives patients the best possible results. In other words, it’s one thing to talk the talk; it’s now time rheumatologists walk the walk. According to Dr. Khanna: “So many groups in healthcare talk about the importance of the patient perspective, but we created a platform to give patients a physical voice. This isn’t an abstract distillation. This is the native voice of truth coming from the source.”
Health Care Provider Training Program Improves RA Care on Navajo Nation
At a presentation, researchers described a new program that offers RA training to primary care providers in the Navajo Nation, the largest American Indian reservation in the United States.* Despite the high prevalence of RA and associated morbidity and mortality in this Indigenous community, the Navajo Nation has a single rheumatologist serving 250,000 tribal members. As a result, most RA care has shifted to primary care providers on the reservation, who do not feel confident prescribing RA medications or managing the disease.
In addition to developing the RA training program, known as the Rheumatology Access Expansion Initiative, researchers wanted to understand how the program affected health care provider knowledge and in RA diagnosis and management.
“The United States faces a critical shortage of rheumatology providers, and this deficit is expected to worsen dramatically over the next decade. In addition, racial and ethnic minorities, particularly Black, Latinx, and Indigenous people, often face longer delays in diagnosis and treatment and [have] less access to rheumatology care,” explains the study’s lead author, Jennifer Mandal, MD, an assistant professor at the University of California, San Francisco (UCSF).
Dr. Mandal says for many patients the physical distance from the nearest rheumatologist is a significant barrier. Meanwhile, many primary care providers have no choice but to attempt to diagnose and treat inflammatory arthritis with little or no specialist guidance.
The 12-week training program was designed by a team of rheumatologists, pharmacists, and Navajo cultural interpreters. It is based on an established educational model, which uses videoconferencing to conduct seminars with community providers. Participants included 15 physicians plus a nurse practitioner, physician assistant, and community health worker.
“We successfully designed and implemented a 12-week RA training program for Navajo Nation primary care providers. The curriculum, now in its third generation, has been very well received and has improved the health care providers’ knowledge of evidence-based RA guidelines and their confidence in disease management,” Dr. Mandal says.
Future plans include expanding the program to other Native American communities and potentially developing a new course on ankylosing spondylitis. The researchers also intend to look at patient outcome data, but “given the history of medical exploitation of American Indians, it is important to us to establish a solid track record of trust and reliability in the Navajo community for several years before we ask permission to review patient health records.”
*Press release: Primary Care Provider Training Program Improves RA Care on Navajo Nation
New Guideline Introduces Recommendations for Integrative Approach to RA Treatment
The American College of Rheumatology (ACR) released its first guideline about an integrative approach to RA. Out of the 28 recommendations, five were about exercise, 13 about rehabilitation, three about diet, and seven about additional integrative interventions. The one “strong” recommendation states that consistent engagement in exercise is advised over no exercise. The type of exercise, frequency, intensity, and duration is not formally defined, but the guideline emphasizes “moving regularly.” The specific elements of an exercise intervention should be tailored to each patient at the given time in their disease trajectory, considering their capabilities, access, and other health conditions.
“Together with pharmacologic treatment options, exercise, rehabilitation, diet, and additional integrative interventions are considered as potential adjunctive treatments for RA. Patients and clinicians often seek evidence-based insight into these treatment options,” said Benjamin J. Smith, DMSc, PA-C, DFAAPA, Interim Program Director and Associate Dean at the Florida State University College of Medicine and co-principal investigator of the guideline. “Recognizing the need to support patients and clinicians when considering treatments to complement their pharmacologic regimen, the ACR developed this guideline.”
Importantly, the guideline recommendations relate to RA-specific outcomes. For example, the guideline recommends adherence to a Mediterranean-style diet over no formally defined diet. The Mediterranean-style diet emphasizes the intake of vegetables, fruits, whole grains, nuts, seeds, and olive oil; moderate amounts of low-fat dairy and fish; and limits added sugars, sodium, highly processed foods, refined carbohydrates, and saturated fats.
“The conditional recommendation for adhering to a Mediterranean-style diet but not other formally defined diets, to improve RA-specific outcomes, may be surprising to some clinicians,” said Bryant R. England, MD, PhD, Associate Professor of Rheumatology and Immunology at the University of Nebraska Medical Center and one of the guideline’s co-principal investigators. “The Voting Panel acknowledged, however, that other health indications may exist for alternative diet and dietary supplements, which makes it crucial for clinicians and patients to engage in shared decision-making.”
The Patient Panel, which provided input into the guideline recommendations, emphasized that rheumatologists are often the first contact for therapeutic decisions. It’s important to patients that their rheumatologists be knowledgeable about integrative therapies and help guide patients to other members of the interprofessional care team with relevant expertise (such as occupational therapists, physical therapists, dietitians, etc.).
“Being able to include the diverse integrative interventions in the management of persons with RA throughout their disease course, as an interdisciplinary team, is essential. This guideline highlights the vital role expert members of interprofessional healthcare teams serve in providing optimal care to people with RA,” said Dr. Smith.
Holding Methotrexate for One Week after Flue Vaccine May Be as Effective as a Two-Week Hold
Methotrexate (MTX) remains a first-line therapy for rheumatoid arthritis due to its efficacy, favorable safety profile and cost. Yet it significantly reduces response to flu vaccines. Previous research has showed that withholding MTX for two weeks after patients received the seasonal flu vaccine improved immunogenicity. New research presented at the ACR annual meeting looked at whether a one-week hold of MTX was equally effective in terms of immediate and long-term vaccine response.
Jin Kyun Park, MD, Chief of Rheumatology at Seoul National University Hospital, associate professor at Seoul National University College of Medicine, and the study’s lead author, says the main reason for undertaking the trial was to determine whether the time without MTX could be minimized to reduce the likelihood of disease flares.
Dr. Park’s team found that discontinuing methotrexate for one week after seasonal influenza vaccination provided the same seroprotection as a two-week discontinuation period in patients with rheumatoid arthritis.*
“Patients and physicians alike do not often know what to do with methotrexate when a vaccination, including the annual flu vaccine or novel COVID-19 vaccines, is required. It was relieving to find out that skipping methotrexate for one week is as effective as skipping it for two weeks to improve vaccine response with no increase in disease flare risk,” Dr. Park says. “But it is not clear yet whether skipping methotrexate for one week improves response to other vaccines.”
The next step, Dr. Park says, is to see if this approach can be applied to other DMARDs and vaccines.
Opioids Double Risk of Venous Thromboembolism in RA Patients
Pain management is a priority for most patients living with RA. Even with well-controlled disease, around 60% of patients continue to experience pain, with few safe medication treatment options, including nonsteroidal anti-inflammatory drugs (NSAIDs) and opioids, to help manage it. One concern with NSAIDs is the increased risk of major cardiovascular events, which is already present in patients with RA. And while many potential harms of opioids — addiction, overdose, and death — are well known, the risk of major adverse cardiovascular events is not as clear.
New research presented at ACR Convergence 2022 looked at this cardiovascular risk in RA patients taking opioids compared to NSAIDs and found that adult RA patients starting opioids had twice the risk of venous thromboembolism (VTE) compared to patients starting (NSAIDs).* VTE is a serious, but preventable, condition that occurs when a blood clot forms in a vein.
The study’s lead author, Gulsen Ozen, MD, a rheumatology fellow at University of Nebraska Medical Center commented: “One of the arguments for choosing opioids over NSAIDs is less impact of opioids on cardiovascular disease. However, no data supports that opioids have a safer profile than NSAIDs in addition to their other risks. Therefore, we wanted to investigate cardiovascular risks associated with opioids compared to NSAIDs to show if they are as safe as perceived.”
The study found similar cardiovascular disease risk and somewhat increased mortality risk with opioids compared to NSAIDs. However, researchers also found a two-fold increased risk of VTE in patients taking opioids.
Dr. Ozen notes that opioid prescribing in the rheumatology community decreased before the COVID-19 pandemic but has since ticked up and remains a problem for many patients with rheumatic diseases.
“Addressing pain in patients with rheumatoid arthritis is challenging as it is not always dependent on disease activity,” Dr. Ozen said. “Although we don’t have direct evidence for patients with rheumatoid arthritis, we know from patients with osteoarthritis that chronic opioid use can intensify pain without improvement of function. Our study suggests that opioids can cause significant cardiovascular morbidity and even death in patients with rheumatoid arthritis. We hope our findings can decrease opioid prescriptions for pain in patients with inflammatory rheumatic diseases. We have to remember that pain in inflammatory rheumatic diseases is multifactorial, and we should utilize non-pharmacological methods more often in this patient population.”
*Press release: Major Adverse Cardiovascular Events and Mortality with Opioids versus NSAIDs Initiation in Patients with Rheumatoid Arthritis
Croatia's and Israel's RA Dashboards are now available
November 8, 2022

Croatia’s and Israel’s Rheumatoid Arthritis Dashboards (RA Dashboard) have recently been published on the Global RA Network website thanks to the collective efforts of the Network’s secretariat and member organizations Association Remisija in Croatia and Mifrakim Tz'eirm in Israel. These new issues bring the total number of countries with the online tool to thirteen.
The RA dashboard provides data in an easy-to-use format to help patients and other stakeholders get a better understanding of the status of rheumatoid arthritis care and gaps in models of care in Network member countries in Europe and the Americas. It also allows to monitor and compare care progress between different countries. It is a powerful tool to support advocacy efforts on models of care in these regions.
Visit the RA Dashboard or Advocacy sections of the Global RA Network website to access RA Dashboards and come back regularly to see updates or new country dashboards.
Poster by Israeli association for RMDs patients Mifrakim Tze'irim (עמותת מִפרקים צעירים)
September 28, 2022
The Israeli association for RMDs patients Mifrakim Tze'irim developed the IN MY HANDS arthritis self-management course for members of their association in collaboration with the Association of Arthritis and Rheumatism – Malta (ARAM) and Malta’s Health Ministry, assisted by a grant from EULAR PARE (People with Arthritis / Rheumatism across Europe). A pilot course was successfully held in 2019 and as of June 2022 over 50 members completed the course.
This image presents the syllabus of the course. Please click here to access the poster.
EULAR 2022 highlights
September 27, 2022
New Population-based Studies Show Increased Risk of Dementia and Depression in RA
Growing evidence from observational studies indicates that patients with RA have a higher risk of developing dementia. The occurrence of depression is also increased. New research shows depression is linked to increased mortality in this population. Clinically active RA was also associated with an elevated risk of dementia. Further studies are warranted to identify mechanisms of increased risk of dementia in RA patients.
See news release:
Data support the idea of a treatment window in the pre-arthritis phase of early RA
Currently, methotrexate is initiated as first-line treatment when arthritis becomes clinically apparent with joint swelling. However, disease processes begin long before patients develop symptoms. New research published at the 2022 EULAR Congress in Copenhagen suggest that there is potential for a treatment window in the pre-arthritis early phase of RA, where limitations can be just as severe as at the onset of clinical arthritis. But it is also important to consider people’s socioeconomic factors, which may also have a bearing on progression to inflammatory arthritis.
See news release:
Gaming for Adherence to Medication: Using virtual care in RA
Effectiveness of treatment for RA is limited by inadequate adherence. Medication adherence can be influenced by implicit attitudes of personal medication needs and concerns about adverse events. The GAMER study targeted these attitudes using a serious puzzle game.
See news release:
Global RA Network launches Rheumatoid Arthritis Dashboard
The new advocacy tool identifies gaps in the delivery of RA care and treatment around the world
Copenhagen, June 1, 2022 – The Global RA Network (the “Network”) today launched a new powerful advocacy tool – the RA Dashboard – as part of its initiatives to improve models of care for people with rheumatoid arthritis (RA). Developed in collaboration with leaders from 18 RA patient organizations, the Dashboard presents key data about the disease and the delivery of RA care and treatment in Europe and the Americas.
RA is the most common autoimmune inflammatory form of arthritis and affects approximately one in 100 persons worldwide. RA reduces a person’s quality of life and is one of the world’s leading causes of disability. Despite its prevalence and costs to societies, the RA models of care vary from country to country and many gaps and inequalities exist.
“Improving RA models of care across Europe and the Americas requires collaboration between stakeholders, including patient groups, policy experts, government and industry, alongside robust RA data. The RA Dashboard is an easy-to-use tool for visualizing the current status of RA care and for monitoring progress on key components of a country’s RA model of care,” explains Cheryl Koehn, president, Arthritis Consumer Experts, which serves as the Global RA Network’s Secretariat.
Koehn added: “Several countries in the Network reported not being able to access key RA statistics in their country for the Dashboard. In those countries, governments are either not collecting data on RA or are not making it public. If governments are not collecting and sharing data on people living with RA, they will not know the magnitude of the problems or how to fix them.”
“As we’ve learned during the pandemic, data is the evidence that drives sound health care decision-making. However, in Romania, nobody knows exactly how many RA patients there are and what RA’s socio-economic cost is. RA data that is accessible in Romania is often extrapolated from general European data but may actually not reflect the actual numbers in our country,” explained Rozalina Lapadatu, president, Asociației Pacienților cu Afecțiuni Autoimune in Romania. Accessible via the Network’s website at https://globalranetwork.org/ra-dashboard, the Dashboard is currently available for 10 countries. The Dashboard data have been researched and collected by member associations and the Network’s Secretariat using local publicly available literature and existing open data sets of government agencies and research organizations as well as results from the Network’s international survey on models of RA care.
“The Dashboard provides an immediate picture of RA in a country like Italy and how our RA care system fares in comparison to other countries in Europe. No standardized RA model of care exists today in Europe or the Americas. This disparity leads to frustration and disappointment for RA patients whose very lives depend on getting a timely and accurate diagnosis, timely access to rheumatologists, and adequate reimbursement for medications, among other critical elements of an effective RA model of care,” commented Antonella Celano, President of Associazione Nazionale Persone con Malattie Reumatologiche e Rare (APMARR) in Italy. “For example, we’ve found 17% of RA patients in Italy waited more than three months for a first visit with a rheumatologist which is significantly above the recommended time between referral and first appointment with a rheumatologist of no more than four weeks.”
People are encouraged to join the conversation about RA, the need for more data about RA and improved RA models of care on Facebook and Twitter @GlobalRANetwork and by using #RADashboard.
About the Global RA Network
Founded in 2016 by rheumatoid arthritis patient organizations and leaders from 18 countries, the Global RA Network was formed to build international relationships and identify and work on common goals and initiatives to improve the lives of people living with RA around the world. The Global RA Network developed a survey that was launched in 2017 called: “Patient experiences of rheumatoid arthritis models of care: An international survey.”
The first crowd-sourced research of its kind designed by RA patients to better learn what their care experiences are like in their country, the global survey highlights self-reported gaps and delays in all five key elements of a standardized RA models of care, including significant delays to diagnosis and specialist access in the countries surveyed, patients not meeting their arthritis specialist often enough, and the need for education/information to increase patients’ confidence to describe RA and improve their ability to care for themselves.
To learn more about the initiatives of the Global RA Network, visit https://globalranetwork.org.
Media contact:
Isabelle Troïtzky – Program Manager, Secretariat of the Global RA Network
Mobile: +1 (514) 220-0085
Email: secretariat@globalranetwork.org
Kelly Lendvoy – Vice President, Communications & Public Affairs, ACE and member of the Secretariat, Global RA Network
Mobile: +1 (604) 379-9898
Email: lendvoy@jointhealth.org
ACR Key RA research takeaways – 2021
December 13, 2021
This year’s American College of Rheumatology’s annual scientific meeting, which took place November 1 to 10, included more than 2,000 abstracts and expert presentations from over 320 clinicians, researchers, and health experts. More than 14,000 rheumatology professionals and patients from 110+ countries attended the virtual conference online.
Here are some key RA research updates:

Rituximab increased odds of COVID-19 hospitalization vs. DMARDs for RA patients
Patient use of rituximab compared with conventional synthetic disease-modifying antirheumatic drugs was associated with worse COVID-19 outcomes in patients with rheumatoid arthritis (RA), according to a presenter at ACR Convergence 2021.
“The COVID-19 pandemic led to several questions regarding the safety of DMARDs that patients with rheumatic diseases use for their management,” said Namrata Singh, MD, MSCIFACP, assistant professor at the University of Washington.
Among different DMARDs, rituximab (Rituxan, Genentech) has a unique mechanism of action with depletion of B cells that can last for several months. Dr. Singh and his research team considered this in their study with the aim to shed light on the comparative safety of rituximab compared with other DMARDs in patients with RA.
“Interestingly, in our study, we did not find an association between rituximab use and mortality from COVID-19,” explained Singh. “This contrasts with a few other studies that did observe an association. We speculate that this could be because prior studies did not adequately adjust for COVID-19 treatments, especially those used during COVID-19 hospitalization, as we did in our analyses.”
No DMARD use was also found to be associated with significantly higher odds of hospitalization in patients diagnosed with COVID-19, according to the study.
“Findings from our study can guide patients, providers and policymakers regarding the increased risks associated with rituximab use during the COVID-19 pandemic,” the researchers said in the presentation.
The data also highlight the need for continued close monitoring of patients on rituximab, the need for COVID-19 vaccination and boosters, and continuation of the other preventive measures, including masking, social distancing and avoiding unnecessary travel.
Black and Hispanic RA patients have higher disease activity than white patients
New research presented at the ACR annual meeting found that racial and ethnic disparities for disease activity persist in people with RA. Black and Hispanic RA patients often had higher disease activity and lower self-reported functional status (basic activities of daily living, e.g., feeding, bathing, dressing personal hygiene and walking) when compared with white patients.
Research has shown that there are differences in disease activity and clinical outcomes for people with RA across different racial and ethnic groups in the United States. These disparities exist across the healthcare system, and these inequities impact both patient experience as well as patient clinical outcomes. However, this has not been studied as extensively in RA as in other disease areas, so there is still a need to understand the magnitude of health disparities in RA. The authors conducted this new study to learn more about these disparities and how they may have changed over time.
According to the presenter of the study, Jacqueline O’Brien, ScD, a clinical epidemiologist:
“The study tells us that, in a population of people who have access to a clinic, have access to treatment, that we’re seeing a lot of differences between the racial and ethnic groups. I think the findings can serve as a reminder to clinicians that it’s important to be mindful that patients are coming from diverse racial and ethnic backgrounds. They may have different needs to achieve similar levels of success with advanced therapy.”
There are many factors that contribute to health inequality, including access to care, socioeconomic status, systemic racism and other social determinants of health (non-medical factors that influence health outcomes).
Dr. O’Brien added. “Certainly, more research is needed to understand how these factors interact and result in different clinical outcomes for racial and ethnic groups. We need to identify where the disparities exist, so that we can better target therapy and improve care, for all patients.”
A key long-term goal is really recruiting diverse populations into future research. RA research has focused predominantly on white populations, and we need more information on the epidemiology of RA (determinants, distribution of diseases), the disease course, the patient reported outcomes in patients of different racial and ethnic backgrounds, and ultimately a complex multifactor solution is going to be needed to address health disparities in RA.”
Going deeper
The underrepresentation of Black, Indigenous People and People of Colour (BIPOC) patients in RA research is a very important finding in and of itself. It suggests that racial minorities are generally being excluded from networks in the arthritis patient community. This means the voices and experiences of BIPOC people living with RA are largely going unheard. This is a particularly significant problem because BIPOC people are more likely to experience negative health outcomes (due to systemic racism) in RA.
A May 2021 study published in Arthritis Care & Research examined 65 ACR and EULAR practice guidelines and recommendations and found a troubling lack of clarity regarding race information, an “urgent need” for standardized race reporting and research with insufficient racial diversity that was used to make race-based recommendations for Black patients.
Higher risk of breakthrough COVID-19 infection in RA, gout, vasculitis patients
Patients with rheumatoid arthritis, gout, vasculitis and those with multiple autoimmune of inflammatory arthritis diseases were at greatest risk for breakthrough COVID-19 infection, despite full or partial vaccination, compared to those without autoimmune disease.
“People with rheumatoid arthritis, gout, vasculitis and multiple autoimmune diseases were significantly more likely to have breakthrough infections compared to people without immunosuppressed conditions,” said Jasvinder A. Singh, MD, MPH, of the University of Alabama at Birmingham, in his presentation at ACR Convergence 2021.
Dr. Sing concluded: “This data, we believe, is important information to guide patients, providers and policymakers. Although more research is needed, these findings support the use of a third vaccination in immunosuppressed patients.”
Vitamin D, omega-3 supplements reduced risk for autoimmune disease, including RA
The use of vitamin D3 or omega-3 fatty acid supplements over a 5-year period may reduce the incidence* of autoimmune disease (including RA) in older adults by 25% to 30%, according to data presented at ACR Convergence 2021.
*(Incidence is a measure of disease that allows us to determine a person’s probability of being diagnosed with a disease during a given period of time. Therefore, incidence is the number of newly diagnosed cases of a disease.)
“In past studies, inflammatory bowel disease, multiple sclerosis and type 2 diabetes have been shown to be more prevalent at northern latitudes, where circulating vitamin D levels are lower,” Karen Costenbader, MD, MPH, director of the Lupus Program at Brigham and Women’s Hospital, told attendees at the ACR meeting. “Both vitamin D and high residential UV exposure were associated with a decreased risk for rheumatoid arthritis among women in the Nurses’ Health Study in our past work.”
However, to date, no prospective randomized trials have tested the effects of vitamin D or omega-3 fatty acid supplementation on the incidence of autoimmune diseases over time, Costenbader noted.
“The reduced incidence of RA is very important for rheumatology,” Costenbader said. “The more pronounced effect after 2 to 3 years of use with vitamin D makes sense biologically and supports long-term use. There is an ongoing extension study confirming incident cases in further follow-up. The clinical importance of these results is very high given that these are well-tolerated, non-toxic supplements, and that there are no other known effective therapies to reduce incidence for autoimmune diseases.”
Glucocorticoid use in RA patients increases cardiovascular risk
According to data presented at ACR Convergence 2021, 30 days of glucocorticoid use in 6 months for RA patients is associated with 15% increased odds of major adverse cardiac events (MACE) in the next 6 months. Glucocorticoids medications are man-made versions of glucocorticoids, which are steroids that occur naturally in your body, and are very effective at reducing inflammation and suppressing the immune system.
“Up to half of RA patients in the United States use long-term glucocorticoids, despite previous work suggesting they increase major cardiovascular events,” said Beth Wallace, MD, MS, of the University of Michigan Medicine and the U.S. Veterans Affairs Ann Arbor Healthcare System.
“Earlier research suggests long-term glucocorticoid use is common among RA patients with traditional MACE risk factors, like hyperlipidemia, diabetes, hypertension and smoking, but we know little about the incremental effect of ongoing glucocorticoid use on MACE risk in RA, particularly as traditionally predisposed comorbidities might confound its assessment.”
Dr. Wallace added: “For example, RA patients who take steroids may be more likely to develop diabetes or hypertension, which, if not adjusted for, could confound an association between glucocorticoid exposure and MACE.”
The study results saw that just 30 days of glucocorticoid use in a 6-month period, even if discontinuous, is associated with a 15% increase in odds of MACE over the following 6-month period. This association appears not to be related to a patient’s baseline MACE risk, or to biologic and methotrexate use.
Key rheumatoid arthritis presentations from EULAR 2019
September 20, 2019
The Annual European Congress of Rheumatology 2019, hosted by the European League Against Rheumatism (EULAR), featured more than 14,500 attendees from 120 countries coming together to hear the best in rheumatology research and clinical advances. The scientific programme included presentations carefully selected from 4,900 abstracts submitted.
This week, EULAR published it’s The EULAR 2019 Report providing the highlights of some of the best presentations, focusing on the clinical and therapeutic findings that are able to change the way rheumatologists and other health professionals practice medicine.
How does it relate to the work of the Global RA Network?
As part of the work of the Global RA Network, our members have defined key elements of a RA model of care that address the complex, life-long issues facing patients and include all points of contact across the health care system.
At EULAR 2019, numerous presentations were related to the Global RA Network’s RA models of care key elements during the patient’s disease journey:
- Global RA Network Model of Care element: Medical Management
As defined by the Global RA Network, the management of RA is complex and requires consistent and frequent monitoring with an arthritis specialist to ensure the effectiveness of treatment and care.
Here are some highlighted EULAR research presentations on “medical management” for RA patients:
EULAR revises its RA management recommendations
The most notable recommendations to RA management discussed at the EULAR conference include:
- no change to designating methotrexate as the first disease-modifying medicine to prescribe, before any biologic medicine;
- no adoption of imaging criteria to determine whether a patient is in remission; and
- no preference is to be given to biologic DMARDS over target synthetic DMARDS
Read more about EULAR revisions to RA management recommendations here: https://www.eularcongressnews-digital.com/eularcongressnews/eular_2019_report?pg=9#pg9
Understanding why some RA patients do or don’t respond to methotrexate. Some newly diagnosed RA patients respond well to the disease-modifying drug methotrexate and others do not. Preliminary EULAR research found that there were differences in how bacterial genes functioned in people who did and did not respond to methotrexate. More research is needed to validate this work and to see whether the model applies to other patient populations. But the research does provide “the first step toward predicting methotrexate response in new-onset RA patients,” according to EULAR Congress News. See the abstract of the oral presentation: https://ard.bmj.com/content/78/Suppl_2/133.3
New JAK inhibitor gets closer to RA approval. JAK inhibitors are targeted oral medications that can treat inflammatory autoimmune diseases. Phase III clinical trial results for a new JAK – filgotinib – were presented at EULAR. The data showed that filgotinib helped prevent radiographic progression and improved physical function among RA patients who didn’t respond to methotrexate. More patients who took filgotinib achieved an improvement of at least 20 percent in American College of Rheumatology criteria (ACR20) after three months compared with patients on a placebo. “Its effectiveness and ease of use make it a potential monotherapy,” said investigator Bernard Combe, MD, PhD, from Montpellier University in France. He predicted that the drug could be on the market within two years. See the abstract of the oral presentation here: https://ard.bmj.com/content/78/Suppl_2/77.3
It may be safe to taper prednisone in RA patients doing well on tociluzumab (Actemra). A new trial found that more than two-thirds of RA patients in remission or with low disease activity who tapered prednisone down to 0 mg/day over the course of six months while taking tociluzumab did not experience disease flares or experience adrenal issues (which can happen while weaning off steroid medication). “Tapering glucocorticoid treatment with an aim for complete discontinuation is worth considering for all patients once they achieve disease control in line with treat-to-target recommendations,” Gerd R. Burmester, MD, director of the department of rheumatology and clinical immunology at Charité-Universitätsmedizin Berlin and Humboldt University of Berline, said in the EULAR Congress News. See the abstract for the oral presentation: https://ard.bmj.com/content/78/Suppl_2/84
It may be safe for RA patients doing well on tofacitinib (Xeljanz) to taper methotrexate. RA patients taking the JAK inhibitor tofacitinib (Xeljanz) plus methotrexate who achieved low disease activity may be able to stop taking MTX without worsening their disease activity. “These results may be used to inform treatment guidelines regarding optimal approaches for discontinuation of methotrexate in patients with rheumatoid arthritis,” study author Stanley Cohen, MD, of the University of Texas Southwestern Medical Center in Dallas, told MedPage Today.
Disease remission associated with 80% reduction in risk of cardiovascular outcomes in RA patients
RA patients who are in remission are 80 percent less likely than those with active RA to have a heart attack or stroke or develop congestive heart failure, according to new Italian research that analyzed data on nearly 900 patients. This is very encouraging news for patients who hear and worry about various RA complications because it indicates that controlling disease activity can reduce the impact of systemic inflammation on other organs. It also highlights the importance and the challenge of getting more RA patients into remission in the first place. Read more about the research: https://www.eular.org/sysModules/obxContent/files/www.eular.2015/1_42291DEB-50E5-49AE-5726D0FAAA83A7D4/03_abstract_op0090_atherosclerosis_in_ra_final.pdf
Preventing gum disease may help manage RA symptoms. A large Japanese survey of rheumatoid arthritis patients found that those with periodontitis (inflammation of the gums) had significantly higher disease activity scores, worse physical function, and greater rates of infection than patients without gum disease. “Oral care is important for patients with rheumatoid arthritis because it appears to improve disease outcomes in clinical settings,” according to Ryoko Sakai, MD, of Tokyo Women’s Medical University, in EULAR Congress News.
- Global RA Network Model of Care Element: Shared Care
As defined by the Global RA Network, treatment decisions should be made through agreement between the patient and the healthcare team, and there must be adherence to the treatment regime.

Here are some research results presented at EULAR 2019 that focus on “shared care” for RA patients:
Patient-healthcare provider relationship key factor if patients take methotrexate as prescribed. Serbian researchers found that patients were more likely to be “non-adherent” to methotrexate if they reported needing better communication with their doctor about RA treatment. About one-third of patients in the study were considered non-adherent to MTX. Patients have many questions about taking methotrexate. It may be the case that improving doctor-patient communication could alleviate some patient concerns. View the abstract here: https://ard.bmj.com/content/78/Suppl_2/1677.1
Doctors working with patients to manage their fatigue. In a session at EULAR titled “My Joints Hurt and I’m Overwhelmingly Tired: Fatigue in Rheumatoid Arthritis”, doctors reviewed how to recognize, assess, and treat fatigue in inflammatory arthritis patients.
“Fatigue remains a difficult-to-address patient concern,” says Maria Danila, MD, a rheumatologist at the University of Alabama Birmingham, who attended the session. Fatigue affects 40 to 80 percent of patients with rheumatic and musculoskeletal diseases, so it was encouraging to see clinicians making this topic front and center at EULAR 2019. See the speaker abstract: https://ard.bmj.com/content/78/Suppl_2/15.2
Doctors helping patients are making exercise a key part of the treatment plan. In a session at EULAR called “Exercise: More Than a Wonder Drug”, attendees discussed “how to help and motivate patients to make [exercise] a habit so they can reap its long-term rewards.” Rheumatologists were advised that although their time with patients is limited and focused on assessing disease activity and reviewing medication management, they should also find the time to encourage physical activity with their patients. See the speaker abstract: https://ard.bmj.com/content/78/Suppl_2/16.5
- Global RA Network Model of Care Element: Patient Self Care
As defined by the Global RA Network, the RA patient should be fully educated about their medical conditions and the importance of closely following the treatment regime.
Here are some EULAR research highlights on RA patient self-care:
Obesity and smoking could be leading factors in RA patients not achieving remission in the first year of treatment. Canadian researchers sought to understand which factors contributed to RA patients receiving guideline-based care not achieving remission in the first 12 months of treatment after being diagnosed. They found that obesity in women and current smoking in men “were the strongest predictors of not achieving remission in the first 12 months” followed by non-use of methotrexate, higher baseline inflammation and longer symptom duration. Researchers suggested that lifestyle interventions such as “smoking cessation in men and weight reduction in women, and optimising methotrexate use may facilitate rapid reduction of inflammation, an essential goal of treatment in early RA.” Read the abstract: https://ard.bmj.com/content/77/Suppl_2/103.2
Mediterranean diet may help RA patients, but more research is needed. There’s scant evidence to support specific diet recommendations to prevent or manage inflammatory arthritis, but many nutrition experts advise patients to follow a Mediterranean-style diet because of other data that links this style of eating to lower risks of heart disease, type 2 diabetes, and certain cancers. One French study from EULAR found that following a Mediterranean diet helped lower the risk of developing rheumatoid arthritis in women who used to smoke. An Italian study found that among people already diagnosed with RA, there was a correlation between following a Mediterranean diet and lower disease activity, although it was not statistically significant. Adhering to the Mediterranean diet was linked with lower rates of high blood pressure and better general health. Read the abstract: https://ard.bmj.com/content/78/Suppl_2/1409





